
Related Posts

YOGA TO REGULATE THE AUTONOMIC NERVOUS SYSTEM
Related PostsYoga,...

IS ALCOHOL A HEALTH FOOD? ALCOHOL AND YOUR HEART
Related PostsWelcome to...

THIS IS YOUR HEART WITH METABOLIC DYSFUNCTION
Related PostsWelcome to...

METABOLIC HEALTH IS MORE IMPORTANT THAN WEIGHT LOSS
Related PostsWelcome to...
SHOULD YOU WEAR A CONTINUOUS GLUCOSE MONITOR?
Related Posts Many of...

IS HEART DISEASE SIMPLY A FAT HEART?
Related PostsThe most...

METABOLIC DYSFUNCTION AND THE ATHEROGENIC LIPID PROFILE
Welcome to a new series on the CFC blog on metabolic health. Metabolism is the process by which the body converts what we eat and drink and stored fat into energy. This energy keeps our cells functioning and our muscles working. Metabolic dysfunction contributes to just about all forms of chronic heart disease and can show itself as hypertension, elevated blood glucose levels, elevated waist circumference, high triglycerides and LDL cholesterol, and low HDL cholesterol. Left untreated, these conditions can become more severe, leading to a diagnosis of metabolic syndrome. In this series, I’ll discuss the causes and impacts of poor metabolic health, testing and treatment, and lifestyle changes you can make at home. Get more lifestyle and health news in your inbox: sign up for the CFC newsletter.
Read more in this series:
Metabolic Health is More Important Than Weight Loss
This Is Your Heart With Metabolic Dysfunction
Your lipid panel says a lot about your health, and I don’t mean your cholesterol level.
You’ve had a lipid panel, and the results are in. Most often, the focus of your conversation with your doctor will be on whether you have high LDL cholesterol and, if so, whether you should take a statin drug. But this discussion regarding your “cholesterol numbers” will be far more enlightening and useful if you ask about the health of your lipoproteins, the particles that carry cholesterol throughout the body. The amount of cholesterol in your blood has surprisingly little to do with artery health–instead it’s the health and qualities of your lipoproteins that matter.
Lipoproteins are particles in the blood that carry cholesterol and triglyceride. When lipoprotein particles are too numerous, too small, or are damaged by glucose or oxidation, they wreak havoc on your arteries and cause coronary artery disease (CAD). The measurement of cholesterol in your blood, or even the measurement of the LDL cholesterol, doesn’t say much about the health of your LDL particles.
The atherogenic lipid profile
The LDL-C on your lipid profile is the amount of cholesterol carried in LDL particles. Sometimes, elevated LDL cholesterol is a sign that those particles are unhealthy. But there are times that the amount of LDL cholesterol can be normal when particles are unhealthy. There are also times that LDL cholesterol is high when the particles are healthy.
The LDL cholesterol is an unreliable predictor of heart disease because a larger number of smaller particles can carry a normal amount of cholesterol. Similarly, more cholesterol can be carried in fewer larger particles. It’s the size and number of particles that are important, not the amount of cholesterol.
When I look at a person’s lipid profile, I look for evidence of an atherogenic (CAD-causing) lipid profile. An atherogenic lipid profile is a sign that there are an increased number of smaller LDL particles. It is atherogenic because a high number of smaller particles are more likely to enter the wall of heart arteries and cause atherosclerosis, coronary artery disease.
I also look for evidence of genetic, lifestyle, and environmental effects on LDL cholesterol that promote heart disease, but the atherogenic pattern is one of the most common and most important to identify.
The atherogenic lipid profile is caused by metabolic dysfunction, a condition that can start with high insulin levels and progress in severity all the way to diabetes.
An atherogenic lipid profile doesn’t come from eating cholesterol, fat, or even saturated fat. It comes predominantly from eating carbohydrates in the form of sugar, especially fructose, and processed foods. These substances make LDL particles smaller, more numerous, and less healthy.
Identifying the atherogenic lipid profile and recognizing its relationship to metabolic dysfunction is important because dietary changes will make the LDL particles larger and healthier.
The triglyceride ratio
You get small LDL particles because the triglyceride carrying particles made by the liver, VLDL (very low-density lipoprotein particles), interact with HDL and LDL particles in the blood stream.
Metabolic dysfunction generates a lot of triglycerides that need to be exported from the liver to be stored in fat tissue. In the blood stream, the various lipid-carrying particles all interact, exchanging cholesterol and triglycerides between them. When the particles start off carrying extra triglyceride, the exchange process results in a lower number of HDL particles and a larger number, but smaller size, of LDL particles.
Metabolic dysfunction results in high triglyceride levels and decreases HDL cholesterol levels. A lipid panel represents this as a high TG/HDL ratio. The amount of triglyceride is higher relative to the amount of HDL cholesterol.
An elevated TG/HDL ratio is an important finding. It is a stronger predictor of coronary artery disease than cholesterol measurements.
I’m suspicious of metabolic dysfunction and atherogenic LDL particles when TG/HDL is higher than 1.8. A ratio of 2.5:1 is abnormal and a TG/HDL ratio >3.5 means atherogenic LDL particles are very likely.
Why small LDL particles cause big problems
The smaller the LDL particle, the more likely it is to enter the artery wall.
The more particles there are, the more likely that they will enter the artery wall and cause damage.
Smaller particles are not as easily removed from the circulation by receptors on the liver, so they linger longer in circulation. Cholesterol medications like statins and PCSK9 inhibitors work by increasing LDL receptors on the liver, so you can help these medications work better by increasing the LDL particle size.
The longer life of small LDL particles explains why there can be so many of them. A longer life also exposes the particles to more oxidation, which makes them even more damaging to the artery wall. A longer life in the blood stream also provides more opportunity for glucose molecules to attach to the particles, further increasing the ability of the LDL particles to attract inflammatory cells into the artery wall.
Metabolic dysfunction is a very common cause of atherogenic lipid profile, but there are other problems that elevate LDL cholesterol that overlap and confuse the picture. These include genetic problems, stress, and inflammation.
Advanced lipid testing
Additional testing can help sort out this complexity.
The simplest and least expensive of these is a measurement of ApoB. An ApoB (apolipoprotein B-100) is present on every LDL particle. Measuring ApoB is like counting the LDL particles. It provides a more accurate measurement of CAD risk and provides information that guides treatment because it can help sort out the genetic and environmental issues that cause abnormalities on the lipid panel.
There are also lipid NMR (nuclear magnetic resonance) tests that measure the number and size of LDL and HDL particles directly.
ApoB and lipid NMR tests may or may not be covered by your insurance. Always ask about the cash price of these tests if your insurance does not cover them. The cash price may be less than the insured cost. It could be worth it to you to pay the cash price if you are motivated to do something with your diet and lifestyle that is specific to your situation.
The atherogenic lipid profile is just one sign of metabolic dysfunction. Metabolic dysfunction is present if you have a diagnosis of diabetes or if you have three or more of the features of metabolic syndrome. These features are elevated TG, low HDL, high blood pressure, increased waist circumference, and elevated blood glucose. But metabolic dysfunction can be present long before diabetes or metabolic syndrome shows itself.
Signs of metabolic dysfunction
To identify metabolic dysfunction, start with the lipid panel, TG/HDL ratio, and ApoB, then look for additional findings that suggest the presence of metabolic dysfunction.
- Measure your waist circumference to see if you are accumulating fat inside the abdomen. Ideally it should be no greater than 32” for women and 36” for men. A waist circumference over 35” for women and 40” for men is a clear sign of excess visceral fat and metabolic dysfunction.
- Ask yourself if you are fatigued, get hungry if you don’t eat frequently, or have a hard time exercising on an empty stomach. These are all signs that you have lost metabolic flexibility, which means your body uses glycogen from food for fuel and has trouble using stored fat. That is the beginning of metabolic dysfunction.
- Ask your doctor to order a HbA1c test to measure your average blood sugar. If your HbA1c is over 5.6 you are prediabetic, but metabolic dysfunction can start with an HbA1c over 5.0.
- An alanine aminotransferase test (ALT) over 25 could mean fatty liver is developing because of metabolic dysfunction.
- A ferritin (iron) level over 150, a hs-CRP (inflammation) over 1.0, or a uric acid level more than 5.5 can be signs of metabolic dysfunction.
- The gold standard test of metabolic health is the oral glucose tolerance test (oGTT), especially when insulin levels are measure along with blood glucose levels.
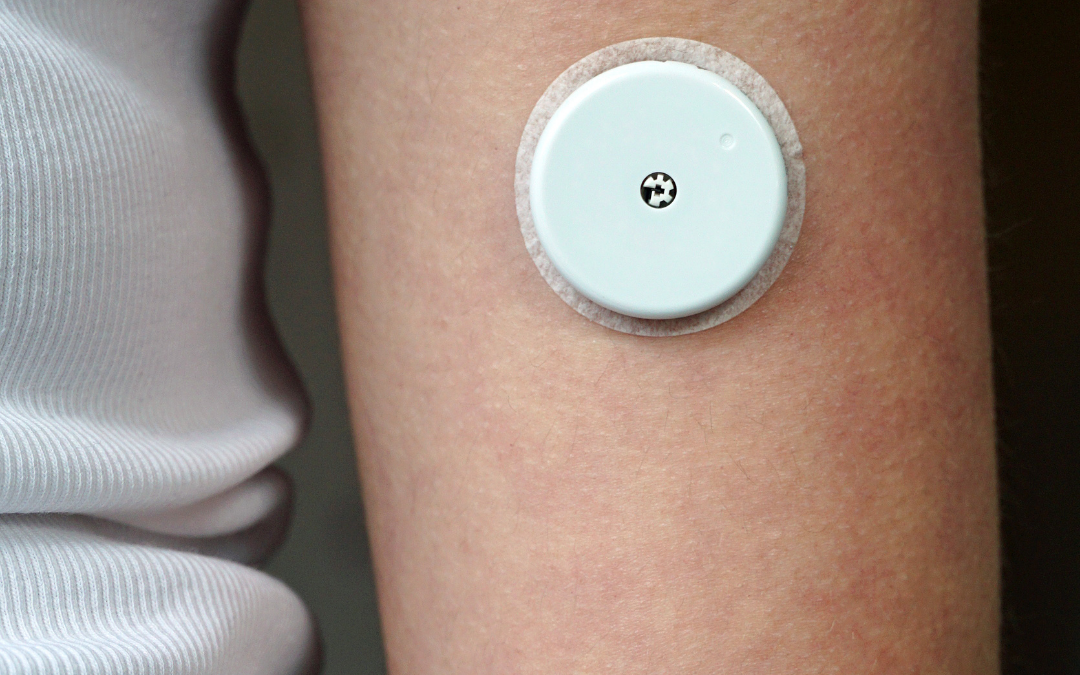
- A continuous glucose monitor like a Libre Freestyle can tell you if your glucose levels rise too much with meals in real life measurements
Metabolic health improves heart health
Metabolic dysfunction and an atherogenic lipid profile are correctable. The cure doesn’t require drugs so much as it does diet and lifestyle changes, such as:
- whole, real, minimally processed foods
- a low-carbohydrate or ketogenic diet
- fasting
- exercise and strength training
- stress reduction
- good sleep
- and a healthy microbiome
Not only is metabolic dysfunction a common problem, it exacerbates the effects of other causes of heart disease. For example, people with familial hypercholesterolemia or combined familial hyperlipidemia have increased risk of coronary artery disease complications when metabolic dysfunction and an atherogenic lipid profile are superimposed. Even in these cases, restoring metabolic health is a priority.
Now you know that an atherogenic lipid profile is more important than elevated cholesterol, and that metabolic dysfunction is the cause of the atherogenic lipid profile. You know how to find out if you have metabolic dysfunction and you know that simple changes in the diet can help it.
The next time you get a lipid panel, ask your doctor, “Do I have an atherogenic lipid profile?” It will tell you much more about your health than simply looking at the LDL number.
