Related Posts

YOGA TO REGULATE THE AUTONOMIC NERVOUS SYSTEM
Related PostsYoga,...

IS ALCOHOL A HEALTH FOOD? ALCOHOL AND YOUR HEART
Related PostsWelcome to...

METABOLIC DYSFUNCTION AND THE ATHEROGENIC LIPID PROFILE
Related PostsWelcome to...

THIS IS YOUR HEART WITH METABOLIC DYSFUNCTION
Related PostsWelcome to...

METABOLIC HEALTH IS MORE IMPORTANT THAN WEIGHT LOSS
Related PostsWelcome to...

IS HEART DISEASE SIMPLY A FAT HEART?
Related PostsThe most...

SHOULD YOU WEAR A CONTINUOUS GLUCOSE MONITOR?
Many of our patients struggle with diabetes or wanting to lose weight. Others are dealing with heart problems, or simply trying to optimize their health. They often ask if they would benefit from wearing a continuous glucose monitor. Short answer? Yes. If there’s just one piece of data you could monitor to gauge overall health, it would be your blood glucose (or blood sugar).
Doctors commonly use fasting blood glucose as a measure of metabolic health, but it’s not a very accurate test. Last night’s meal, the quality of your sleep, and the stress and activity of your morning can throw off the measurement—it’s a snapshot, not a full picture. A somewhat better picture of your metabolic health comes from an HbA1C test. This test tells us your average blood glucose over the past three months by measuring how much glucose is attached to your hemoglobin molecules. (Hemoglobin is the part of red blood cells that carries oxygen from your lungs to the rest of your body.)
But the HbA1c test can sometimes be misleading. The amount of glucose that attaches to hemoglobin depends on how long your red blood cells (RBCs) live in your blood stream. On average their lifespan is 3 months, so if those cells have a shorter life span than average, your A1C reading will be inaccurately low. And people with atypically long-lived red blood cells will have HbA1c measurements that suggest higher blood glucose than they really have.
The blood glucose continuum
Conventional wisdom says that if your HbA1c measurement is above 6.5, you have diabetes, and if it’s below 5.6, you’re healthy.
The first problem with these definitions of health and disease is that average blood glucose elevations exist on a continuum. The ideal HbA1c is really less than 4.8. If average glucose rises above that level, there can be long term health consequences, like diabetes and heart disease. By the time your HbA1c averages 5.6 or 6.5, your metabolic health is already at risk without lifestyle steps to manage it.
It’s important to remember that blood glucose goes up whenever we eat. Beyond looking at average blood glucose, if you want a clear picture of your metabolic health, it is important to know how your blood glucose behaves in response to the foods you eat. High spikes and variability in your blood glucose readings reflect insulin spikes that damage your health and cause heart disease and aging.
Measuring glucose after a meal
An excellent test to measure your metabolic health is the oral glucose tolerance test (OGTT) with insulin measurements. The OGTT measures your blood glucose and insulin response to a specific amount of glucose. Because it measures the variability in glucose, the OGTT provides information about your metabolic health not provided by HbA1c.
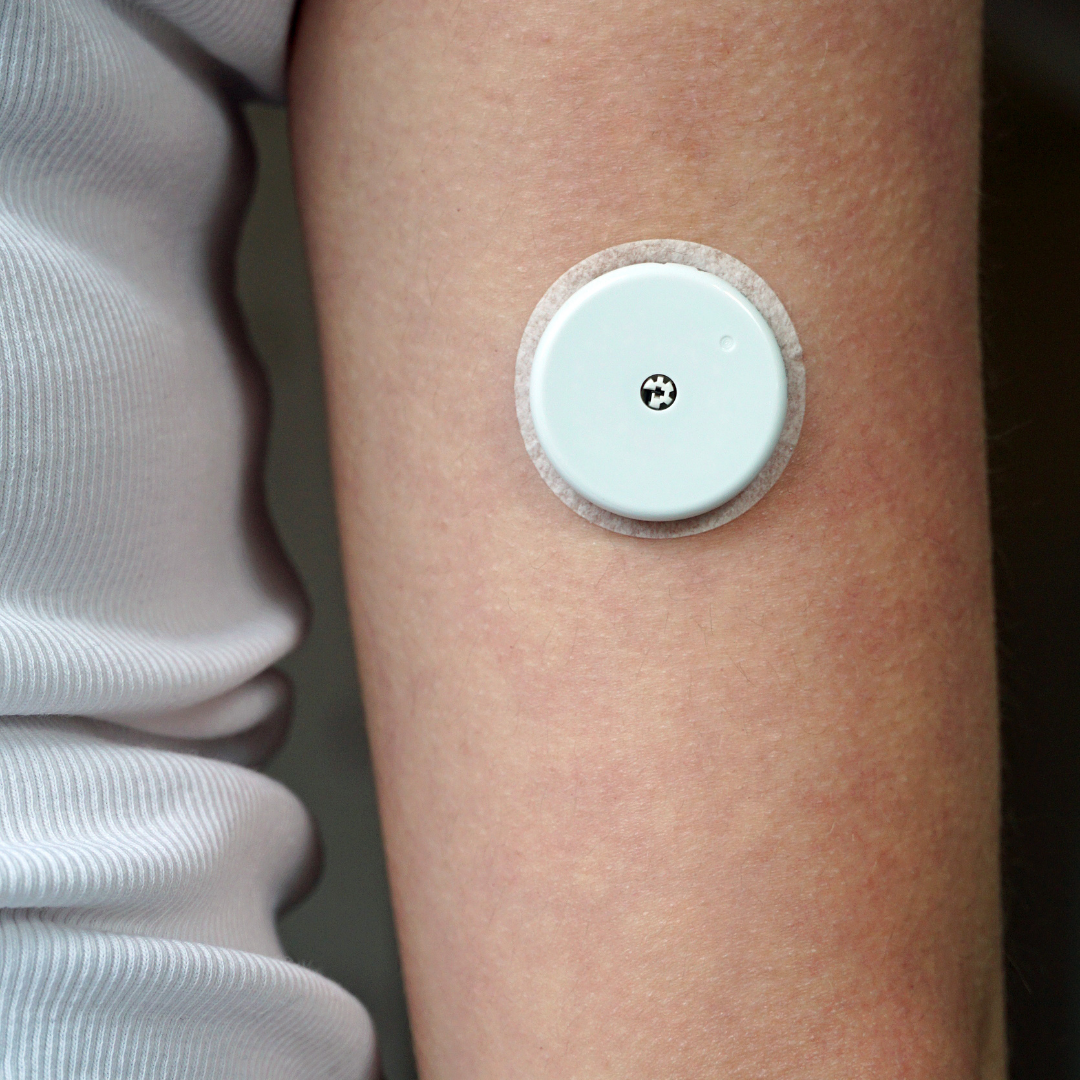
While you can partially simulate an OGTT by measuring your blood glucose periodically after a meal with a finger pricking device, continuous glucose monitors (CGM) are a more convenient tool to help you accomplish your metabolic health goals. CGM devices, such as the Freestyle Libre, use a sensor placed on the back of your arm that gives a graph of your continuous glucose readings, visible on an app on your phone. Typically, the CGM is worn for a two-week period to accurately troubleshoot the impacts of your diet and lifestyle.
More than what you eat
Food isn’t the only thing that affects your blood glucose. Your physiologic state also determines your insulin and glucose response. Blood glucose goes up during a workout, but overall, exercise reduces your glucose response to food. And, crucially, poor sleep and chronic stress raise blood glucose.
What should your blood glucose goals be?
You want to minimize your average blood glucose–but what is a healthy reading? Average glucose readings < 100 are the goal and correspond to a good HbA1c of 4.8 to 5.1.
For post-meal blood sugar spikes, you want to reduce–and hopefully eliminate–peaks above 140. And dips below 70, hypoglycemia, predict increases in appetite and indicate large insulin swings.
Meal composition, carbohydrate intake, and portion size all affect blood glucose readings. So do sleep, stress, and exercise. One of the best ways you can improve your metabolic health is to understand the impact of your diet and activities. If you want to improve your health, talk to your doctor about wearing a CGM. It may help you lose visceral fat, manage your diabetes, and even heal your heart.
Practical information for using a CGM
CGM sensors such as the Libre Freestyle require a prescription from your physician. Unless you have diabetes and use insulin, it isn’t covered by insurance. The sensor costs approximately $65 and records blood glucose for 2 weeks.
The sensor records the glucose in the interstitial space outside of fat cells in your skin, not in your blood. The accuracy of the sensor is +/- 13% compared to blood glucose. Accuracy may be lower the first and final days of wearing it.
To use the sensor, place it on the lower half of the back of your upper arm. It should be low enough to show if you’re wearing a short sleeve garment. The sensor does not hurt and sticks well even with showering.
You’ll need a scanner or you can use your smart phone (such as iPhone 6 or later) with the Libre Freestyle app to view the data your sensor records. A graph showing up to 6 hours of glucose data is downloaded to the app when you make a recording. Since the sensor can only store 6 hours of data it must be scanned or synced with your app frequently. I recommend taking recordings right before bed, first thing in the morning, and after each meal.
The FDA-approved indication for CGM sensors is to monitor insulin therapy. The CGM will warn you of high and low blood sugar readings relevant to diabetic patients taking insulin. If this is not why you’re using a CGM, the warnings and recommendations for insulin therapy may not be relevant to you.
Make sure that while you’re wearing the sensor, you’re keeping a complete diary of your food intake, activity, sleep quality, and stress levels. With your diary and sensor data you can make lifestyle and diet changes that optimize your glucose variability.
You want to shoot for an average daily glucose < 100 and post meal peak glucose < 140.
You may get the information you need to optimize your glucose response with one 2-week sensor, or you may want to repeat to gauge how your glucose is responding to medications and lifestyle changes.
Aim for optimal, not just OK
As we now know, metabolic heath exists on a continuum. Evidence shows that lower glucose is better for cardiovascular health and overall survival. What should your optimal goals for health and longevity include?
- Fasting glucose on CGM, during sleep, is optimal at 72-85 mg/dl.
- Your baseline glucose before a meal should be 72-90 mg/dl.
- The best post-meal glucose response is a rise of glucose less than 30 mg/dl, and never higher than 110 mg/dl.
- Your optimal average daily glucose should be in the range of 79-100 mg/dl.
Learn more: watch the webinar “Should You Wear a Continuous Glucose Monitor?”
