
Related Posts

YOGA TO REGULATE THE AUTONOMIC NERVOUS SYSTEM
Related PostsYoga,...

IS ALCOHOL A HEALTH FOOD? ALCOHOL AND YOUR HEART
Related PostsWelcome to...

METABOLIC DYSFUNCTION AND THE ATHEROGENIC LIPID PROFILE
Related PostsWelcome to...

METABOLIC HEALTH IS MORE IMPORTANT THAN WEIGHT LOSS
Related PostsWelcome to...
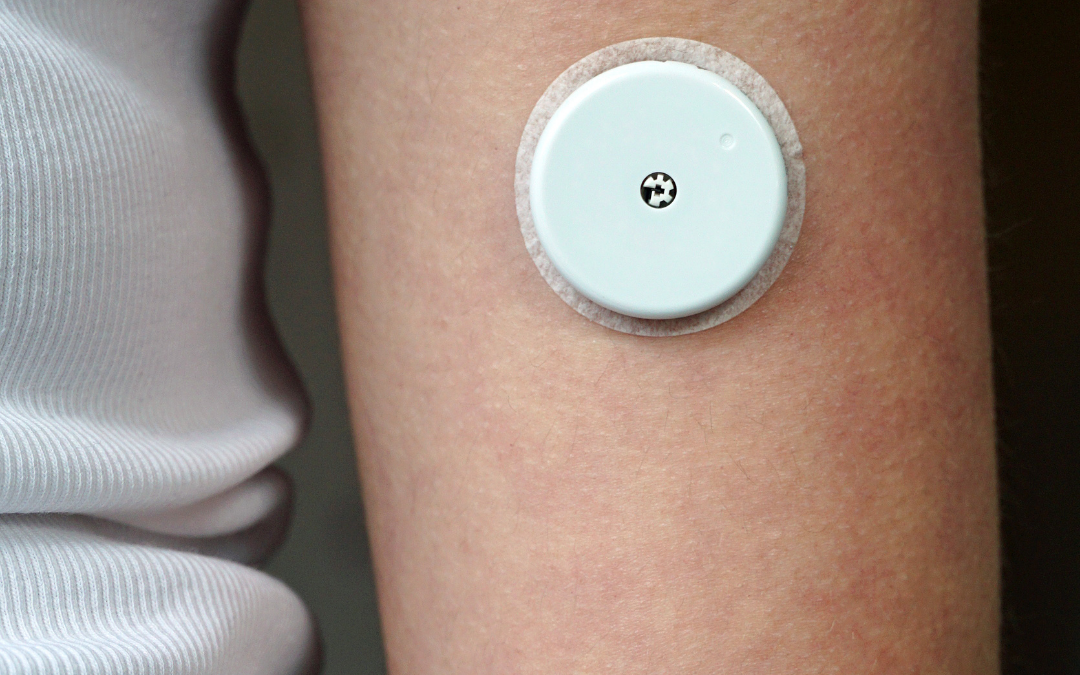
SHOULD YOU WEAR A CONTINUOUS GLUCOSE MONITOR?
Related Posts Many of...

IS HEART DISEASE SIMPLY A FAT HEART?
Related PostsThe most...

THIS IS YOUR HEART WITH METABOLIC DYSFUNCTION
Welcome to a new series on the CFC blog on metabolic health. Metabolism is the process by which the body converts what we eat and drink and stored fat into energy. This energy keeps our cells functioning and our muscles working. Metabolic dysfunction contributes to just about all forms of chronic heart disease and can show itself as hypertension, elevated blood glucose levels, elevated waist circumference, high triglycerides and LDL cholesterol, and low HDL cholesterol. Left untreated, these conditions can become more severe, leading to a diagnosis of metabolic syndrome. In this series, I’ll discuss the causes and impacts of poor metabolic health, testing and treatment, and lifestyle changes you can make at home. Get more lifestyle and health news in your inbox: sign up for the CFC newsletter.
Read more in this series:
Metabolic Dysfunction and the Atherogenic Profile
Metabolic Health is More Important Than Weight Loss
Fat on the heart inflaming your atrium, ventricle, and coronary arteries; damaged LDL cholesterol particles penetrating the wall of your heart arteries; heart muscle cells starving for energy; constricted and clotted arteries. What metabolic dysfunction does to your heart and blood vessels is not pretty.
Previously, I discussed how focusing on metabolic health can help heal your heart. Today, we’re describing in graphic detail how metabolic dysfunction causes heart and vascular problems. I hope to motivate and empower you to do something about it.
Where metabolic dysfunction begins
Insulin is the hormone responsible for, among other tasks, pushing glucose and fatty acids into muscle cells. Metabolic dysfunction begins when the chemical pathways that allow glucose and fatty acids to enter the cell are impaired. Without these substates for energy creation, the muscle is starved. A compensatory increase in the level of insulin hormone will allow more glucose to enter the cell, but not fatty acids, so your body is still deprived of energy.
This compensatory increase in insulin levels is called insulin resistance (IR). Insulin resistance is progressive. Over time, your body needs more and more insulin to support glucose metabolism, and elevated insulin levels cause a lot of damage. You may be diagnosed with Type 2 diabetes when glucose levels become high enough.
The problems of insulin resistance with poor cellular energy production, increasing insulin levels, and increasing glucose levels also have far reaching effects on the heart and blood vessels.
Metabolic dysfunction deprives the muscles and heart of energy
For the most part, glucose and fatty acids, which are the basic fuels your body uses to produce cellular energy, must be actively transported into muscle cells. The earliest signs of metabolic dysfunction are a shift from fatty acid oxidation to glucose metabolism, meaning that your body is using glucose (sugar) instead of fat for fuel.
A respiratory quotient (RQ) test measures the ratio of carbon dioxide produced to oxygen consumed. In a metabolically healthy state, the RQ is 0.7, meaning that fatty acid metabolism is dominant. An RQ above 0.8 toward 1.0 indicates dependence on glucose metabolism and poor metabolic health.
A healthy athlete uses little glucose for fuel at rest and can generate cellular energy from fat up to very high workloads. People with metabolic dysfunction are fueled only by glucose. When you can’t utilize fatty acids, physical exertion becomes more difficult. The inability to metabolize fatty acids makes exercise difficult, especially when fasting, when the body has depleted glycogen stores. Fatigue and exercise intolerance are common symptoms of metabolic dysfunction. The heart muscles also experience fatigue with metabolic dysfunction, which can cause heart failure.
Elevated insulin levels drive visceral fat accumulation
In addition to pushing glucose into muscle cells, insulin also regulates fat storage. Elevated insulin gives the signal to store energy in fat cells and not to release it. Elevated insulin levels make it harder to use the energy our bodies have stored in visceral fat. As visceral fat accumulates, it becomes a source of inflammation. Visceral fat that accumulates around the heart is called epicardial fat. If you have too much epicardial fat it can damage the atrium, leading to atrial fibrillation. It can damage the ventricle, leading to heart failure. Epicardial fat also covers the coronary arteries and makes artery plaque more prone to rupture and heart attack.
Elevated insulin causes high blood pressure
Insulin also causes salt retention in the kidneys. This leads to salt sensitive hypertension. Restricting salt intake is recommended if you have high blood pressure. But I like to correct the root of the problem: high insulin, which causes salt sensitivity. You can read more about that here.
Metabolic dysfunction makes LDL particles more atherogenic
Excess glucose must go somewhere if it can’t be used by your muscles, so the liver transforms excess glucose into triglycerides (TG). The newly made triglyceride, along with some cholesterol, is packaged into water-soluble particles that are carried in the blood and stored in fat cells. In the bloodstream, these triglyceride-rich VLDL (very-low-density-lipoprotein) particles take some cholesterol from HDL cholesterol particles, and they become small LDL particles.
Metabolic dysfunction causes a characteristic “atherogenic lipid profile” in lipid testing. This profile consists of an increased level of triglyceride relative to a decreased level of HDL cholesterol. The ideal TG/LDL ratio is 1.0. The higher the TG/LDL ratio is above 1.8, the more likely you have increased numbers of LDL particles, and the more likely those particles are small. Advanced lipid testing and ApoB measures the number and size of LDL particles. Small, damaged LDL particles are associated with coronary artery disease more than is elevated cholesterol. I’ll explain this in more depth in a future post.
Elevated insulin damages arteries
Increased insulin levels damage the endothelial, or inner, lining of arteries. This reduces the production of chemicals like nitric oxide (NO) that relax the arteries, resist blood clotting, and inhibit inflammation. The result is endothelial dysfunction with constricted blood vessels, increased clotting, and inflammation of the vessel wall. Insulin is also a growth-stimulating hormone that encourages growth of atherosclerotic plaque.
Insulin causes oxidative stress
Insulin resistance stimulates oxidizing enzymes and inhibits antioxidant enzymes. The blood vessels are damaged by oxidative stress, which is the accumulation of oxygen free radicals. Oxygen free radicals cause DNA and cellular damage.
High blood glucose damages arteries directly and through the immune system
Eventually, metabolic dysfunction leads to high levels of glucose: first after meals, and then persistently. Excess glucose attaches to proteins in the blood and on the endothelial lining of blood vessels. This attachment can change the function of the protein or alter it so much that the immune system thinks it is a foreign substance that needs to be attacked. When immune cells attack the artery wall and atherosclerotic plaque, plaque rupture and heart attack are more likely.
The effects of metabolic dysfunction are working on your heart even before a diagnosis is made of diabetes, prediabetes, or metabolic syndrome. Wherever you are on the spectrum of metabolic dysfunction, your heart will benefit by moving back toward metabolic health.
Read more on the CFC blog on epicardial fat and fasting with heart disease to learn what you can do to improve your metabolic health.
