
Related Posts

ARE YOU DEFICIENT IN OMEGA-3 FATTY ACIDS?
Related PostsRecently,...

WILL FISH OIL HELP OR HURT YOUR HEART?
Related PostsOmega-3...

EARLY ABLATION FOR ATRIAL FIBRILLATION: IS IT BETTER THAN LIFESTYLE MODIFICATIONS?
Related PostsIn my...

GARLIC HERB BUTTER ROAST CHICKEN
Related PostsThis...

ONE-PAN MEDITERRANEAN BAKED FISH
Related PostsThis...
THE FUTURE OF PLAQUE IMAGING & DIAGNOSING CORONARY ARTERY DISEASE
Related PostsWhat is...
IS YOUR GUT THE CAUSE OF YOUR HEART DISEASE?
Related PostsAt...

BRUSSELS SPROUT HASH WITH ROASTED MUSTARD SEED AND WHITE FISH
Related PostsI love to...

BREAKING (AND ENTERING) A FAST: TWO DELICIOUS SOUP RECIPES
Related PostsWe’re...

NATURAL WAYS TO DO WHAT STATINS DO
Related PostsStatin...
CARDIOVASCULAR DRUGS AND POTENTIAL NUTRIENT DEFICIENCIES
Related PostsCommon...
TREATING ATRIAL FIBRILLATION WITH ACUPRESSURE
Related PostsAtrial...

HEALTHY RECIPES FOR A CROWD
Related PostsUpdated...

ABLATION AND BEYOND FOR ATRIAL FIBRILLATION
Should your ablation come with a warranty?
As a functional cardiologist, I apply my knowledge of functional medicine and cardiology to make it less likely that an ablation would be necessary for myself or any patient with atrial fibrillation. If an ablation were necessary, I would apply all my skill and knowledge to be sure it would be effective.
I wish the same for you. I want you to understand how atrial fibrillation happens and how ablation can help it. Ablation is often an important but incomplete treatment for AF, and personalized lifestyle medicine should be part of the solution, whether you get an ablation or not.
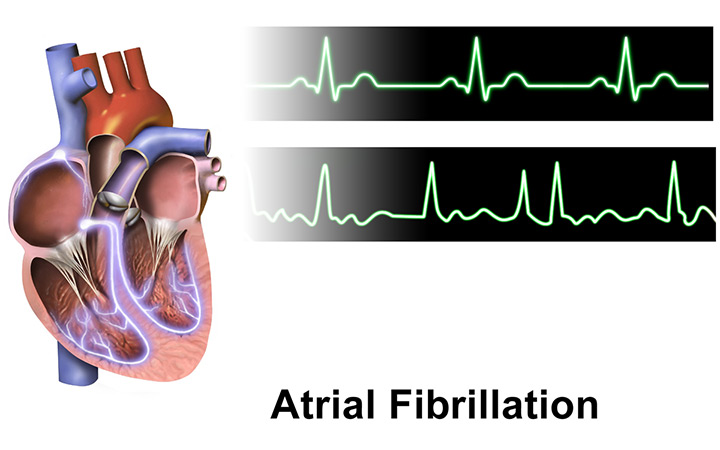
Understanding atrial fibrillation (AF)
Atrial fibrillation is more than a change in the heart rhythm. The irregular pulse that characterizes atrial fibrillation is a sign that an atrium of the heart is sick.
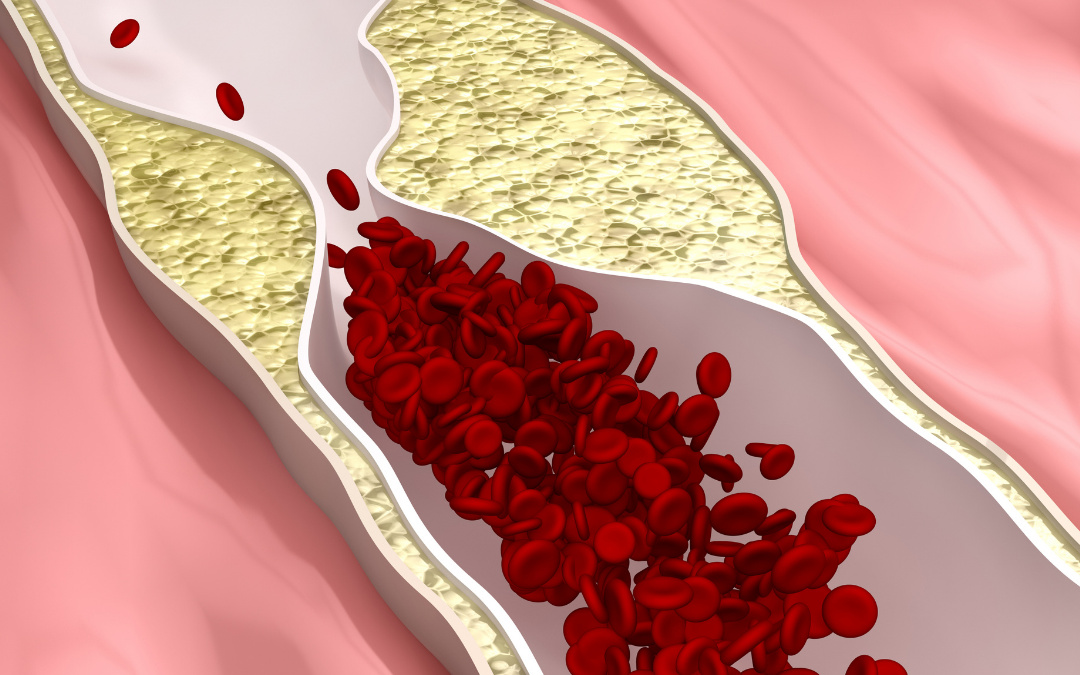
When our hearts are beating normally, an electrical impulse originates in the right atrium and flows through both atria heart chambers. The electrical impulse enters into the ventricles, which pump blood to the lungs and body. Atrial fibrillation occurs when the electrical conduction through the atrial chambers gets broken up into multiple wavelets that conduct chaotically. The electrical signals in the atrium flow into the ventricles and produce a chaotic heartbeat (usually too fast.) So, the first treatment for atrial fibrillation is usually a medication to slow down the pulse.
The breakup of electrical signals in the atrium can occur when the atrium is damaged and when it is stressed by the occurrence of rapidly occurring extra triggering electrical signals. The damage in the atrium makes electrical signals prone to break up. Surprisingly, the triggering electrical signals come from the veins that connect the lungs to the back of the left atrium. These are called pulmonary vein triggers.
What is ablation?
Ablation works by preventing the pulmonary vein triggers from entering the atrium.
To perform an ablation, small catheters are inserted into the veins of the legs which lead to the heart. These are used to deliver heat or cold to the atrium, create scar tissue, and blocks the electrical signals which trigger atrial fibrillation from entering the atrium. This ablation procedure is called a pulmonary vein isolation (PVI).
Heating of the tissue is called radiofrequency (RF) ablation. Cooling of the tissue is called cryoablation.
Ablation can be simple or complicated
Paroxysmal atrial fibrillation episodes start and stop on their own. People who have atrial fibrillation episodes that occur infrequently and go away quickly are likely to have many pulmonary vein triggers and may not have a very damaged atrium. Ablation with PVI works best for these people.
Those with longer, more frequent, or persistent episodes of atrial fibrillation that don’t stop on their own typically have more damage or scarring of their atrium. Ablation with PVI alone does not work as well when the atrium has more damage. A more complicated ablation that includes heating or cooling of the scarred areas of the atrium in addition to PVI is often performed when people have persistent atrial fibrillation.
The complexity of an ablation can also go up because other abnormal heart rhythms, atrial flutter and atrial tachycardia, are common in people who have atrial fibrillation. ECGs and ambulatory monitoring are needed to show the atrial fibrillation and any additional heart rhythm problems.
More advanced atrial fibrillation and more arrhythmias mean a more complex ablation and a greater chance of something going wrong or not working.
Ablation relieves symptoms from atrial fibrillation
The symptoms and consequences of atrial fibrillation can be very different from person to person. For some, atrial fibrillation is barely noticeable, while for others, an irregular or racing heartbeat can be very disturbing. For many people, fatigue and shortness of breath with exercise are most disturbing.
When a paroxysm of atrial fibrillation begins, the heart rate often jumps up uncomfortably. Doctors commonly prescribe medications to slow the heart rate during atrial fibrillation, and this can help a lot. This is called “rate control.” Medications intended to prevent or stop episodes of AF are called “rhythm control.” A cardioversion is a procedure used to convert persistent atrial fibrillation to normal rhythm with an electrical shock.
In some people a combination of rate control, rhythm control, and cardioversion therapies does the job and that is all they need to feel close enough to normal. In others, residual symptoms or side effects prompt consideration of an ablation.
Ablation is good for reducing symptoms. Even when atrial fibrillation is not cured by an ablation, it may occur less often and cause fewer symptoms.
Ablation provides a great benefit to symptomatic people with atrial fibrillation by restoring a normal heart rhythm. Even when atrial fibrillation recurs after an ablation, the episodes can be less frequent and shorter in duration. For a time, symptoms of atrial fibrillation are at least reduced, if not eliminated, after an ablation. There is some evidence that complications of atrial fibrillation are partially reduced by ablation.
Does ablation cure atrial fibrillation?
From the beginning, ablation was intended as a curative therapy for atrial fibrillation. In order to receive FDA approval of ablation equipment and to receive reimbursement from payors, a high bar for success was needed.
While ablation works to control atrial fibrillation when drugs don’t work, and while ablation also reduces symptoms more effectively, it does not “cure” atrial fibrillation. The closer you look for small episodes and the longer you wait after an ablation, the more atrial fibrillation you find. After 3 years have passed, half of people see problems with atrial fibrillation recurring.
Ablation doesn’t cure atrial fibrillation because it doesn’t fix the sick atrium.
The success of an ablation also depends on how sick the atrium is. More ablations are performed for people with paroxysmal than persistent atrial fibrillation because the outcomes are better. If you have a sicker atrium, consider carefully whether the ablation procedure is likely to help, and have realistic expectations.
Atrial fibrillation is a progressive problem
As AF worsens, the atrium becomes more damaged, and the duration and frequency of atrial fibrillation episodes increase; the abnormal rhythm can even become persistent. As the atrium becomes sicker, the risk of complications increases, including stroke, dementia, heart failure, and death.
Because atrial fibrillation itself can damage the atrium and lead to more frequent or prolonged episodes–“atrial fibrillation begets atrial fibrillation”–ablation has been thought to reduce AF progression.
But ablation does not treat the reason that the atrium is sick in the first place. If fat is building up on the surface of the atrium causes damage to the atrium–epicardial fat–ablation won’t stop it. If there is oxidative stress, inflammation, toxins, autoimmune damage, or pressure build-up stretching the atrium, these factors will continue to damage the atrium after the ablation.
Does ablation reduce the complications of atrial fibrillation?
Stroke is the most feared possible complication of atrial fibrillation. While the average risk of stroke is two and a half times greater with atrial fibrillation, for some people the risk is barely elevated and for others the risk may be much greater.
When the heart rhythm is abnormal, blood flow can be slowed, increasing the risk of clotting and stroke. So why isn’t the risk stroke increased to the same degree in everybody with atrial fibrillation?
It’s because atrial fibrillation episodes are not the main cause of strokes and other complications: the sickness of the atrium, and associated sickness of the endothelial lining of the heart and blood vessels, are the problems. The atrial fibrillation is more of an aggravator.
The sicker the atrium, the slower the blood flow can be during episodes of atrial fibrillation, and the higher the risk of stroke may be. There is also evidence that endothelial dysfunction contributes to the complications of atrial fibrillation.
For example, stroke is more likely to occur during atrial fibrillation, but it can occur whether or not a damaged atrium is fibrillating. So, ablation can reduce, but not eliminate the risk of stroke.
People with atrial fibrillation are also more prone to dementia. There are many potential reasons for this. Studies are ongoing to determine the impact of ablation on this issue.
While the impact of ablation on outcomes is controversial, an exception is in people with a weak heart–heart failure with reduced ejection fraction (HFrEF)–and a lot of atrial fibrillation. For these people, ablation can reduce the burden of atrial fibrillation and improve symptoms and probably even prolong life. This is a situation in which ablation can be very helpful.
Another type of heart failure, heart failure with persevered ejection fraction (HFpEF) commonly occurs in people with atrial fibrillation. This combination of problems is associated with metabolic disease: blood sugar and insulin problems that lead to Type 2 diabetes. HFpEF is characterized by excess epicardial fat. This problem is both common and progressive, and can lead to high blood pressure in the lungs. Ablation is being studied to determine how it affects this condition.
Most ablations are performed for people with paroxysmal atrial fibrillation who have symptoms that limit them in spite of medications. Performing ablation for the purpose of reducing complications is not standard practice, although studies to measure the ability of ablation to reduce complications continue. Any consideration of having an ablation to preempt these complications or to stop blood thinning medications needs to be made with careful estimation of the risks and benefits in consultation with a very experienced electrophysiologist.
How risky is ablation?
I recently learned about the death of an acquaintance. By accounts, he was strong, fit, and healthy. But he had atrial fibrillation. He developed neurologic symptoms and fever, leading doctors to suspect that he had meningitis. Very quickly, his situation deteriorated, and in spite of antibiotics and intensive medical care, he died. This all occurred 2 weeks after an ablation for his atrial fibrillation. This tragic story is consistent with a rare but well described complication called atrial esophageal fistula, which can occur after atrial fibrillation procedures.
The esophagus lies directly behind the left atrium of the heart, leaving it vulnerable to damage during an ablation. In atrial esophageal fistula, contents of the esophagus enter the left atrium, flow to the brain, and cause infection and inflammation that results in symptoms that mimic stroke and meningitis.
The doctor who performed the ablation did not necessarily make a mistake. The possibility of esophageal damage during an ablation is well known and great care is taken to reduce the risk of this devastating complication, but it’s not fully preventable. In spite of precautions, at least one atrial esophageal fistula occurs for every thousand atrial fibrillation ablations performed. I say “at least” because this complication occurs weeks after the ablation and, as in the situation above, may not be recognized and diagnosed.
If I needed an ablation to treat my atrial fibrillation, I would not be deterred by the possibility of this relatively rare problem. This is partly because, as an interventional electrophysiologist, I know it’s unlikely to occur, and partly because I am aware of the possibility and would be watching for symptoms. On the other hand, I would prefer not to have an ablation unless I really needed it.
Complications occur in 5-10% of people who undergo an ablation. Most complications are temporary issues related to placing and removing the catheters in the blood vessels of the legs.
Life-threatening complications like atrial esophageal fistula are rare but real. Since dangerous complications affecting the heart might not show themselves until days or weeks after leaving the hospital, they are often not counted. Real world estimates of mortality up to 30 days after an ablation are 0.5 to 1.5%.
The largest number of life-threatening problems occur in older and sicker patients, but no one is immune from the possibility of damage to the heart, esophagus, blood vessels, lungs, or nerves around the heart.
The experience of the doctor performing your ablation is gigantically important in determining the success and complication of an ablation. Surprisingly, most of the ablation procedures done in the US are performed by operators who do 25 or fewer procedures per year. The success and safety of an ablation is substantially improved when the doctor and hospital do more than 50-100 of the procedures per year.
Are there different kinds of ablation?
Many patients sought me out for ablation because I was one of the first to use a cryoballoon instead of an RF catheter for PVI. The RF catheter delivers energy though its tip to make many “spot welds” around the pulmonary veins. The cryoballoon temporarily freezes the tissue in one shot around the vein and was associated with fewer complications, including less damage to the esophagus. Today, the safety and efficacy of improved RF catheters and cryoballoon catheters are very similar. Less than 20% of people now require a second procedure early on to complete a PVI.
If your doctor thinks additional ablation outside of the pulmonary veins is needed, there are more decisions to make. An experienced operator will make the best choice of catheter to deliver energy and which areas need to be ablated.
Breakthroughs on the horizon
Over the last 20 years, equipment used to perform ablation has evolved and become more sophisticated, and expensive, in an effort to reduce complications. A new type of ablation catheter that uses an energy source called Pulsed Field Ablation holds the promise of performing ablation with lower risk of complications. In particular this catheter may reduce the risk of atrial esophageal fistula. Studies in humans are just beginning, so this type of ablation is not currently available.
Are there alternatives to ablation?
Lifestyle modification can be very effective for atrial fibrillation. 50% of overweight people who lose 10% of their body weight no longer need an ablation.
There are many treatments and lifestyle changes that can reduce atrial damage by addressing underlying causes:
- Reduce epicardial fat through fasting, diet, and exercise
- Treat metabolic dysfunction
- Reduce inflammation, oxidative stress, toxins
- Treat underlying infections, autoimmune problems, sleep problems, and stress
Reducing damage to the atrium can help avoid an ablation, decrease the progression of atrial fibrillation after an ablation, and reduce the risk of complications.
Ablation has not been tested in comparison to personalized lifestyle change.
Not everyone with atrial fibrillation is a candidate for ablation. If evaluation shows the damage to the atrium is already severe, the probability of success is lower and ablation may be inappropriate or too risky.
Ablation and personalized lifestyle change can complement each other
Personalized lifestyle medicine can benefit symptomatic people with atrial fibrillation. These treatments can mitigate the damage to the atrium that leads to progression and complications by treating the underlying causes.
If you have atrial fibrillation, personalized lifestyle medicine can reduce your need for an ablation. If you have an ablation, personalized lifestyle medicine can help make the benefits last longer.
Everyone’s atrial fibrillation is different
Everyone has unique underlying reasons that makes the susceptible to atrial fibrillation. The symptoms of atrial fibrillation and the impact on your quality of life are different. The risk of atrial fibrillation complications is different. Navigating the treatment options for AF can be a very personal choice.
Choosing an experienced electrophysiologist with good judgment is the most important determinant of a good outcome from an ablation. While electrophysiologists are experts at performing ablation, few are experts at evaluating and treating the underlying causes in a holistic fashion.
At Colorado Functional Cardiology, we have the experience and expertise to both treat atrial fibrillation and its root causes. Our approach is to use personalized lifestyle medicine to reduce the complications of atrial fibrillation in a holistic way and add ablation when more treatment is needed.
Try this tip for easing AF symptoms at home with acupressure.
