Related Posts

ARE YOU DEFICIENT IN OMEGA-3 FATTY ACIDS?
Related PostsRecently,...

WILL FISH OIL HELP OR HURT YOUR HEART?
Related PostsOmega-3...

EARLY ABLATION FOR ATRIAL FIBRILLATION: IS IT BETTER THAN LIFESTYLE MODIFICATIONS?
Related PostsIn my...
IS YOUR GUT THE CAUSE OF YOUR HEART DISEASE?
Related PostsAt...

ABLATION AND BEYOND FOR ATRIAL FIBRILLATION
Related PostsShould...

NATURAL WAYS TO DO WHAT STATINS DO
Related PostsStatin...
CARDIOVASCULAR DRUGS AND POTENTIAL NUTRIENT DEFICIENCIES
Related PostsCommon...
TREATING ATRIAL FIBRILLATION WITH ACUPRESSURE
Related PostsAtrial...

THE FUTURE OF PLAQUE IMAGING & DIAGNOSING CORONARY ARTERY DISEASE
What is coronary artery disease (CAD)? What does it mean to you if your doctor says you have CAD? And what does it mean if she says that your heart tests are “normal”?
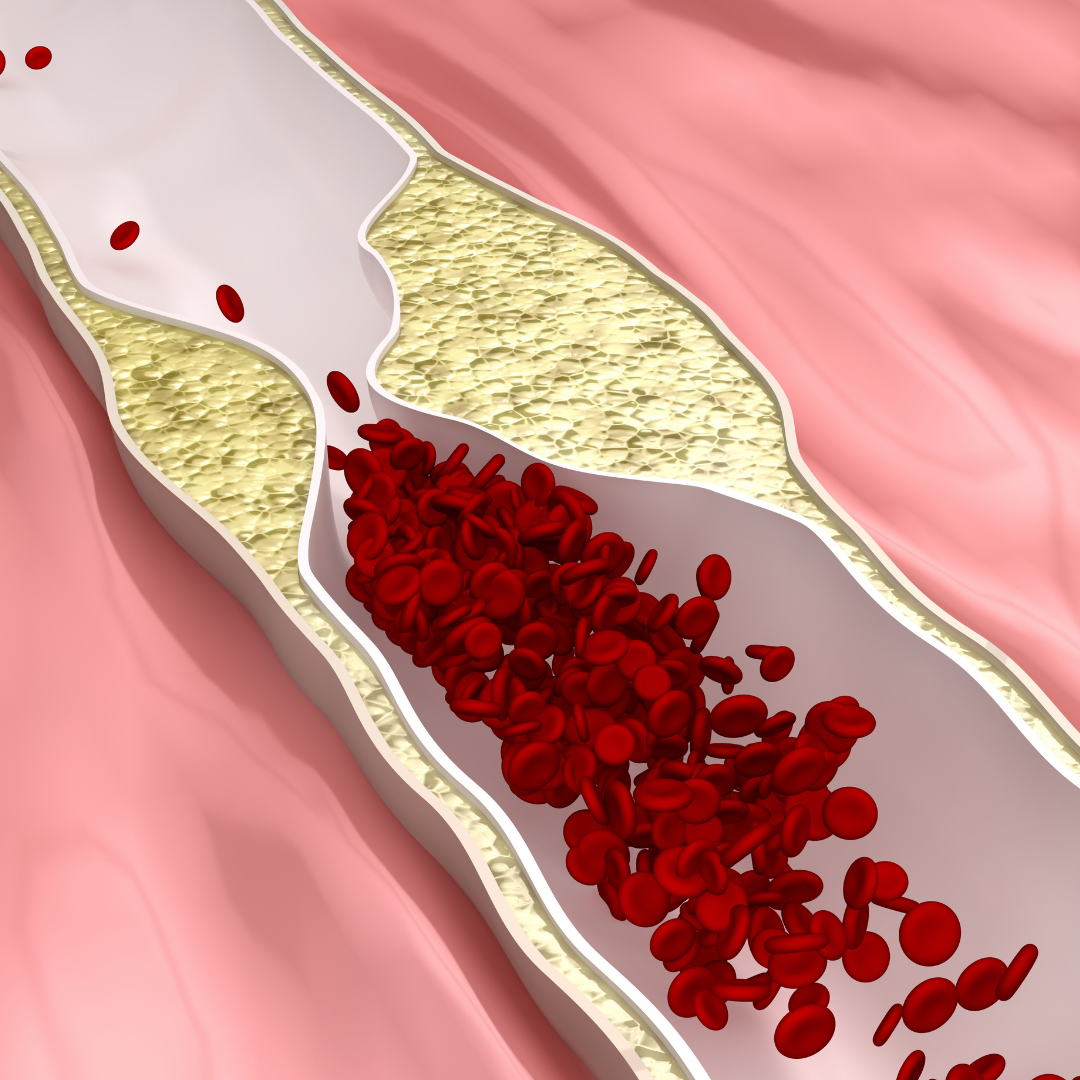
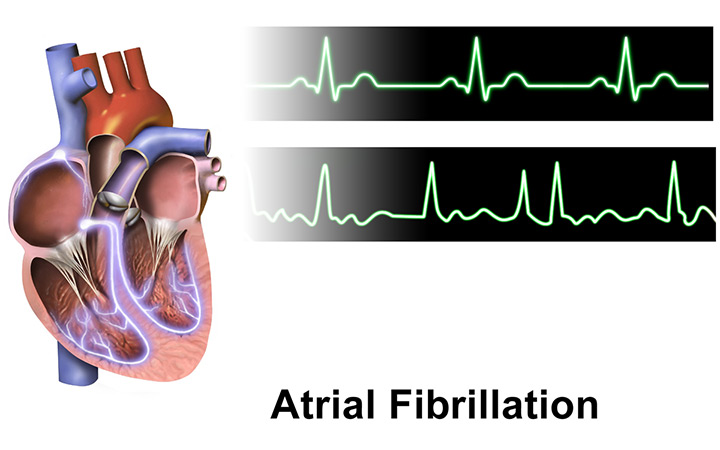
Most people equate CAD with a blocked heart artery (or coronary artery). There are several ways to know if you have a blocked artery. If you’ve had a heart attack, one of your heart arteries was completely blocked by plaque, at least temporarily. If the blockage (or obstruction, in clinical terms) is severe enough to restrict blood flow to your heart muscle, a stress test can diagnose it. A coronary angiogram, or heart catheterization, is designed to detect coronary obstruction of 70% or more.
What is coronary artery disease?
You don’t have to have a blocked artery to have CAD. CAD is present in your arteries long before blood flow becomes restricted and even longer before a heart attack occurs. It can take decades before CAD progresses to these symptomatic levels. It is far better to know you have CAD before a blockage forms in an artery.
CAD exists in the wall of your artery, but it’s not a deposit on the artery wall. It begins slowly, with damage to the internal lining of the artery. This is called endothelial dysfunction, which opens the door to the development of CAD.
What causes CAD?
When you think of heart disease, cholesterol probably comes to mind. But cholesterol is not the cause of CAD. The particles that carry cholesterol around in the body, called lipoproteins, are more the problem, especially when those lipoproteins are damaged. Cholesterol measurements can be a surrogate for the presence of problems with lipoproteins.
Lipoproteins can become damaged from genetic reasons, lifestyle issues, or other medical problems. The problem with damaged lipoproteins is that they attract the attention of your immune system. Macrophages, one type of immune cell, interact with the apolipoproteins inside the artery wall and turn into “foam cells” that become saturated with LDL cholesterol and die.
After your immune system kills something—in this case, the macrophage cells—it begins a process of repair. In your heart arteries, the repair process brings in muscle cells, fibrous tissue, and calcium. Foam cells accumulate and repair progresses to thicken your artery wall. This is coronary artery plaque.
When plaque becomes a problem
Most plaque does not cause blockages in your artery lumen (the hollow passageway that blood flows through). A plaque can be invisible to all the tests we use to diagnose obstructive coronary disease. Plaque can be present in your arteries when your doctor says your heart tests are normal.
A plaque can be invisible, but it can still be terribly destructive. Most heart attacks are caused by plaques that are small and don’t obstruct the artery until they break open. This is called a plaque rupture. When a plaque ruptures, a blood clot forms that can completely and suddenly block blood flow to the heart.
Even a small amount of plaque can be dangerous, and it can cause a heart attack tomorrow or in 30 years. We classify any plaque in your arteries as CAD. Before a heart attack, or before a blocked artery is diagnosed, plaque in an artery means there is coronary artery disease.
Detecting plaque
Since tests for artery blockage don’t detect non-obstructive plaques, we depend on surrogate indicators of their presence. The surrogate measures don’t directly detect plaque, but they can predict the probability of a heart attack—often called a coronary event—happening in the next 5 to 10 years.
Therapies based on surrogate indicators don’t work very well. Worse, the only way to know that therapy is not working is if a heart attack occurs. 70% of heart attacks occur despite therapy. We use traditional coronary risk factors, such as cholesterol, coronary artery calcium, hypertension, smoking, diabetes, and family history, as surrogate indicators. These risk factors can be helpful, but it is better to see directly if plaque is present, how much there is, and to analyze the characteristics of the plaque. Plaque is characterized as calcified, non-calcified, or soft. Soft plaque is the kind that carries the highest risk of a plaque rupture. Plaques that are prone to rupture are called vulnerable or unstable plaques.
Knowing how much plaque is present and what kind it is means we’re able to test new therapies that can reduce it or change its character from vulnerable, heart attack-prone plaque to stable, less dangerous plaque.
The future of plaque imaging
We discover other diseases with imaging. A woman knows if she has breast cancer via a mammogram, breast imaging. If cancer is present, she has imaging to determine the size and extent of the problem. The individual characteristics of the tumor are measured to personalize therapy. She will also have imaging repeatedly to determine the effectiveness of therapy.
When we know plaque is present in your heart arteries, we can move beyond surrogates to definitively identify the plaque. This is a new technology called coronary artery plaque imaging.
Coronary artery plaque imaging is a totally different way of identifying CAD and is completely changing the way we think about heart disease diagnosis and therapy.
The risk of a heart attack depends on the amount and character of plaque present in the artery, not on blockage. With plaque imaging, we can personalize therapy to improve the plaque characteristics. We will be able to tell if therapy is working without waiting for a heart attack to occur to find out it didn’t.
How to image your plaque
Plaque imaging first requires a coronary CT angiogram (CCTA). CCTA is easy to undergo. It only requires an injection of iodine contrast into a vein. CCTA by itself does not image plaque, but when AI algorithms are applied to the images, developed by a company called Cleerly Coronary, the plaque appears.
Plaque has a complicated structure with some features that suggest vulnerability to plaque rupture and others that predict stability. Cleerly shows that character with color coded images. Blue represents stable calcified plaque, yellow is non-calcified plaque, and red is liquified plaque that is most likely to rupture into the artery and cause a heart attack. The Cleerly examination shows how much and what structure the plaque has in each part of each artery. It’s similar to how we measure the stages of cancer. We can repeat CCTA imaging to gauge the effect of statins and other therapies—including lifestyle changes.
If you are interested in Cleerly plaque imaging, it is available but is not currently covered by insurance. The cost of the CCTA varies from $150 to $550 in the Denver area. The cost of the Cleerly examination is an additional $750.
Paradigm shift
Plaque imaging is on the forefront of a paradigm shift. The diagnostic value of plaque imaging will continue to improve, its role in the diagnosis and management of heart disease will evolve, and cost and coverage will catch up with the benefit of this life-saving tool.
Plaque imaging is empowering because it gives you the knowledge you need to motivate and maintain the changes that have the biggest impact on your health.
This is important because heart disease, and particularly CAD, is responsible for more deaths than any other health condition, including all forms of cancer combined. Heart disease also killed twice as many people as COVID-19 in 2020 alone. But 80% of CAD deaths are preventable. Plaque imaging is a tool that may allow us to get ahead of this scourge that grows in our arteries for decades before it kills.
Now if you ask the question, Do I have CAD? there is an answer, which can also answer the next questions: how much? what kind? how dangerous is it? And most importantly, what can I do about it?
Learn more: watch our recent webinar “What’s Growing in Your Arteries?”
