
Related Posts

ARE YOU DEFICIENT IN OMEGA-3 FATTY ACIDS?
Related PostsRecently,...

EARLY ABLATION FOR ATRIAL FIBRILLATION: IS IT BETTER THAN LIFESTYLE MODIFICATIONS?
Related PostsIn my...
THE FUTURE OF PLAQUE IMAGING & DIAGNOSING CORONARY ARTERY DISEASE
Related PostsWhat is...
IS YOUR GUT THE CAUSE OF YOUR HEART DISEASE?
Related PostsAt...

ABLATION AND BEYOND FOR ATRIAL FIBRILLATION
Related PostsShould...

NATURAL WAYS TO DO WHAT STATINS DO
Related PostsStatin...
CARDIOVASCULAR DRUGS AND POTENTIAL NUTRIENT DEFICIENCIES
Related PostsCommon...
TREATING ATRIAL FIBRILLATION WITH ACUPRESSURE
Related PostsAtrial...

WILL FISH OIL HELP OR HURT YOUR HEART?
Omega-3 fatty acids, in the form of fish oil, are a popular supplement for heart health. But there is some controversy over whether they work to prevent heart attacks and whether they increase the risk of atrial fibrillation. Is fish oil a supplement or a drug, and does it help or hurt your heart?
Physicians and alternative practitioners commonly recommend omega-3 fatty acids as “nutraceuticals” to people with inflammatory and autoimmune conditions. Nutraceuticals are pharmaceutical alternatives that are often unregulated or unproven treatments.
Many supplements on the market today are taken without prescriptions, but we think of them as being as effective as medications. When buying a supplement, we should always ask ourselves:
- Am I taking this because I’m deficient?
- How do I know my body will benefit from it?
- How will I know if it’s working?
Treating a person vs. treating a condition
Nutraceuticals (and pharmaceuticals) are often recommended to treat a condition—not a person. I argue that personalized use of nutraceuticals allows for more targeted therapy with better chance of benefit and less of harm. Yes, harm can come from nutraceuticals. When a supplement is used as a medicine the stakes are often lower, but there are still benefits and risks.
What is the difference between treating a person and a condition or disease? Treating a condition implies that the therapy will help all or most people who have that condition. Treating a person requires that we assess why that person’s condition exists and how the therapy may impact it.
The use of omega-3 fatty acids teaches us some lessons about treating persons rather than diseases. Omega-3 supplementation is associated with reduced arrhythmias, inflammation, and autoimmune symptoms. But it has also been associated with some increase in arrhythmias, particularly atrial fibrillation. There is also controversy over the use of omega-3s to lower triglycerides and reduce the risk of heart attack.
The story of omega-3 fatty acids
The story of omega-3 fatty acids illustrates how difficult it is to use supplements to treat chronic diseases. Doctors, dieticians, internet “experts,” and alternative practitioners alike all muddle up the information and make it harder to make sense of. They all focus on the use of these supplements for “conditions.”
The bottom line is that, like any supplement or alternative therapy, you need to know if omega-3s are right for you personally. And you must be able to determine if they are working for you.
Omega-3 fatty acids live in all our cell membranes. They are essential fatty acids, meaning our bodies cannot make them and we need to get them from food or supplements. Some people can manufacture them from alpha linolenic acid (found in nuts and seed oils), but most people get omega-3s from fish or fish oil.
EPA and DHA, two of the fatty acids that make up omega-3s, are both known for their anti-inflammatory properties. They also send signals into the cells that influence multiple chemical pathways. Two of these signals have implications for heart disease. Omega-3s affect the electrical properties of heart cells and influence how fatty acids are released from their storage form, triglycerides.
We can measure the level of omega-3 fatty acids in your body. Some people are deficient, especially if they rarely eat fatty fish, such as salmon, or nuts. The percentage of red blood cell membranes made up of omega-3s is called the Omega-3 Index. People with a low index are deficient in omega-3s and can fix that by changing their diet (more fish) and/or taking a high-quality fish oil supplement.
If a person has inflammation, autoimmune problems, elevated triglycerides, atrial fibrillation, or coronary artery disease, and is deficient in omega-3 fatty acids, it makes sense to correct the deficiency. But if your Omega-3 Index is not low, does it make sense to supplement? It’s difficult to know, because the tests we use to determine if omega-3 supplements are effective rarely measure the Omega-3 Index at baseline. Researchers are not trying to correct a deficiency; they are trying to fix a problem with fish oil that is not caused by a deficiency in omega-3 fatty acids.
Omega-3s for triglycerides and coronary artery disease
Physicians prescribe pharmaceutical-grade EPA to reduce triglyceride levels and prevent heart attacks. This use of fish oil illustrates the problems that can occur when you treat a lab test and not a person. Omega-3 fatty acids will reduce triglyceride levels, but does that mean it will reduce heart attacks? That depends on whether the elevated triglyceride levels cause the heart attack or whether something else causes heart attacks and elevated triglycerides.
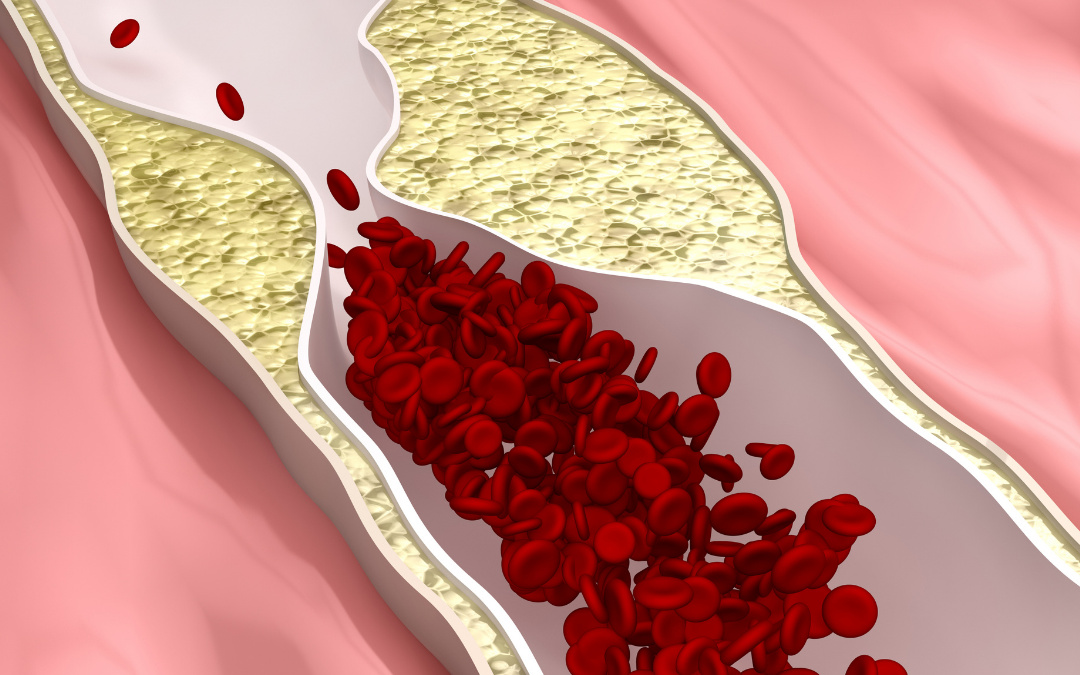
Insulin resistance is a common cause of high triglyceride levels. With insulin resistance, a lot of triglycerides move through the liver into the blood to be stored in fat cells. The triglyceride-rich particles coming out of the liver interact with cholesterol-carrying particles. This reduces the number of HDL particles and elevates the number of LDL particles. These LDL particles are both more numerous and smaller. Small LDL particles damage arteries and cause coronary artery plaque. This is called the atherogenic lipid pattern.
Lowering triglycerides but not correcting insulin resistance
If you’re taking fish oil to reduce the risk of a heart attack, it needs not only to reduce triglycerides but to correct the atherogenic lipid pattern. Omega-3 fatty acids decrease the ability of fat cells and LDL particles to release triglycerides. So blood levels of triglycerides go down, but the amount coming out of the liver is not necessarily reduced. Perhaps this is the reason that clinical trials of pharmaceutical-grade EPA or EPA/DHA are inconsistent in their effects on heart attack risk. They lower triglyceride levels without correcting insulin resistance or the atherogenic lipid pattern that are the root cause of much artery disease.
The error of thinking that reducing triglycerides will reduce heart attack stems from the error of assuming that triglycerides cause artery disease. But an atherogenic lipid profile, not triglyceride levels, are the better surrogate for heart attack risk. This is the same error that comes from using cholesterol blood and not abnormal lipoprotein particle levels as a surrogate for coronary artery disease.
If your triglyceride levels are elevated, the correct response is to investigate the cause. If the cause is insulin resistance, this can be improved by dietary low-carbohydrate therapy and fasting. Treating insulin resistance is a better strategy than taking a nutraceutical that lowers triglyceride levels without fixing the heart-damaging insulin problem. Alcohol use and genetic variants can also be a factor in elevated triglycerides. Lack of fish oil is not likely to be a cause of elevated triglyceride levels, and therefore not the best, or at least not the only, treatment.
Omega-3s and heart arrhythmias
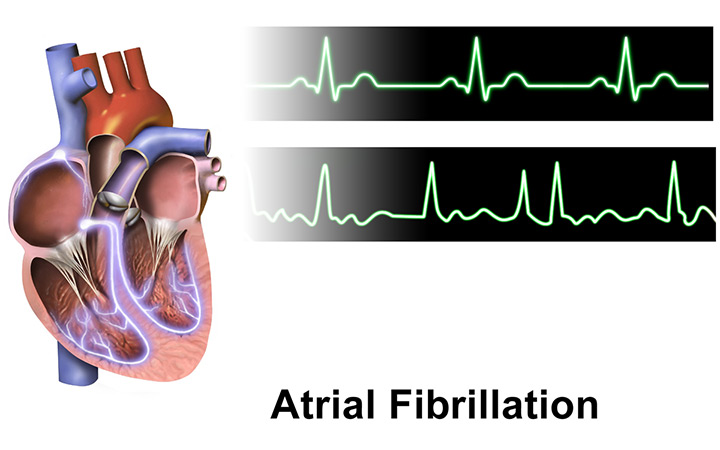
Omega-3 supplements are claimed to be both a cause of and treatment for heart arrhythmias. Recent studies of EPA or EPA/DHA in people with coronary disease have shown an increase in the risk of AF. About 2% of people who are not taking fish oil have atrial fibrillation, compared to about 3% with fish oil. It is not a huge absolute risk, but an impressive relative risk increase.
Understanding the effects of omega-3 fatty acids on the electrical properties of cells helps us to understand this effect. Omega-3 fatty acids can promote calcium buildup in the cells, leading to extra electrical firing. In people susceptible to AF, the extra firing may provoke an episode. In other people, the fish oil may have an electrical stabilizing effect on overactive sodium channels.
Fish oil can increase vagal tone, which in general is good and reduces the risk of cardiac arrest. But in some people with AF, increased vagal tone can increase the amount of atrial fibrillation they experience.
The effect of omega-3s on cardiac arrhythmias will vary depending on the state of your heart’s electrical system before you take them. People who say fish oil is good for heart arrhythmias or bad for heart arrhythmias are both probably right. It is the individual person who determines the effect of fish oil on arrhythmia risk, not the diagnosis.
Personalized approach to omega-3 fatty acids supplementation
If your Omega-3 Index test says you are deficient in Omega-3 fatty acids, it may be a good idea to correct that by eating low mercury fish, taking a supplement, or correcting digestive issues.
If you are taking fish oil empirically (to correct deficiency), a low dose contains around 1 gram (1,000 mg) of combined EPA/DHA. A high dose is around 4 grams.
If you have elevated triglycerides with insulin resistance and an atherogenic lipid profile with numerous small LDL particles and low HDL, look at your diet. Low carb, ketogenic, or fasting techniques can improve your metabolic health. Taking a fish oil supplement is not a magic pill that will fix these issues. There is a difference between eating fish and taking fish oil. Every study of fish consumption suggests an improvement in heart disease outcomes.
If you have atrial fibrillation, you should correct any omega-3 fatty acid deficiency but avoid high dose omega-3 fatty acids. In some people, atrial fibrillation may get worse, and more atrial fibrillation can mean increased risk of stroke.
An elevated hs-CRP in a C-reactive protein test can suggest that inflammation is aggravating your heart condition. If you have any autoimmune condition or chronic inflammation, fish oil can be helpful. But it does not replace identifying and correcting the source of chronic inflammation.
There are practical issues with taking fish oil supplements. Most concerning is the risk that the fish oil you are taking is oxidized (or gone rancid). This is a big problem with low quality or poorly stored fish oil. Oxidized oils will increase your oxidative stress and aggravate heart disease and arrhythmias.
Best plan: eat fish at least 2-3 times per week. Focus on low mercury varieties such as wild salmon, mackerel, and sardines.
Take therapeutic supplements intelligently
Whenever you think that you can take a supplement to treat a disease, think carefully. Things are probably more complicated than you think. Supplements are best used therapeutically in individual people with specific needs. It is less likely that supplements will help if you use them to treat diseases in general or disease surrogates, like an abnormal laboratory test, unless those tests indicate a deficiency.
It is important to work with a professional who can help you to determine if supplementation with EPA or EPA/DHA, or any nutraceutical, is right for your lifestyle, diet, health conditions, and physiology. Ask about measuring your Omega-3 Index, inflammatory markers like hs-CRP and ferritin, fasting insulin, and HbA1. I also recommend getting an advanced lipids panel that includes LDP particle number and particle size.
If you cannot get the type of evaluation you need to be sure that a “promising” nutraceutical is right for you, try it cautiously, be skeptical, and always have a low threshold for stopping it if you suspect any issues. Taking things that you “heard would be good for your condition” is fine when the stakes are low, but when dealing with heart disease it is wise to determine what your body needs.
The temptation to use nutraceuticals as medication alternatives is common. Nutraceuticals are medications. Whether a supplement comes from a drug company or a supplement company (and often they are the same), that alone does not make one better for you than the other. You always need to be aware of the potential risks and benefits, and if that supplement is right for you.
Get more lifestyle and health news in your inbox: sign up for the CFC newsletter.
