Related Posts

ARE YOU DEFICIENT IN OMEGA-3 FATTY ACIDS?
Related PostsRecently,...

WILL FISH OIL HELP OR HURT YOUR HEART?
Related PostsOmega-3...

EARLY ABLATION FOR ATRIAL FIBRILLATION: IS IT BETTER THAN LIFESTYLE MODIFICATIONS?
Related PostsIn my...
THE FUTURE OF PLAQUE IMAGING & DIAGNOSING CORONARY ARTERY DISEASE
Related PostsWhat is...

ABLATION AND BEYOND FOR ATRIAL FIBRILLATION
Related PostsShould...

NATURAL WAYS TO DO WHAT STATINS DO
Related PostsStatin...
CARDIOVASCULAR DRUGS AND POTENTIAL NUTRIENT DEFICIENCIES
Related PostsCommon...
TREATING ATRIAL FIBRILLATION WITH ACUPRESSURE
Related PostsAtrial...

IS YOUR GUT THE CAUSE OF YOUR HEART DISEASE?
At Colorado Functional Cardiology, we’re in the business of finding the root causes of heart disease. If you’re told that your high cholesterol is causing your artery disease, or that you have atrial fibrillation because of high blood pressure, you’re just going around in circles. We must investigate: why is your cholesterol or blood pressure high in the first place?
Inflammation, oxidative stress, autoimmune problems, and metabolic dysfunction damage the heart and blood vessels. These conditions also aggravate cholesterol, drive up blood pressure, and promote atrial fibrillation. But they’re processes that we can get under control by understanding how your genes interact with your environment and lifestyle to cause them.
Your gut may be the root of heart and autoimmune disease
Poor gut function can lead to nutritional deficiencies that promote disease. For instance, hypochlorhydria (low stomach acid): if we have inadequate stomach acid or other digestive enzymes, our gut doesn’t break down food sufficiently to allow nutrients to be absorbed. Inflammatory bowel disease is another condition that prevents absorption of nutrients. Nutrient deficiency and other gut problems can be an important contributor to heart problems.
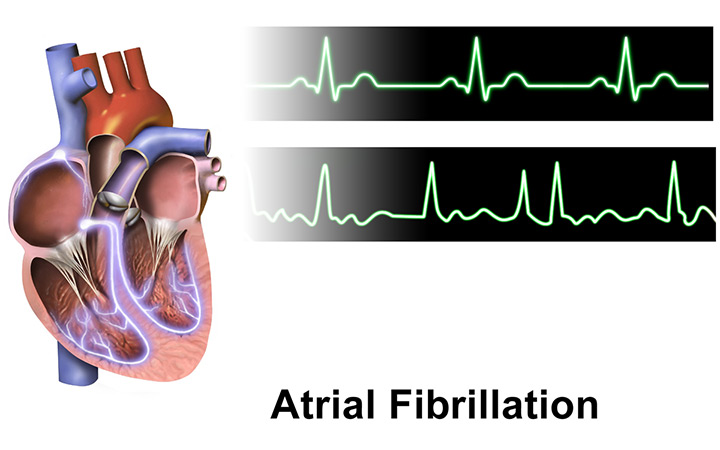
The gut is an important control center of the immune system. Communication between the gut and the brain involves the vagus nerve, which, through a process called vagal tone, regulates heart rate, vasodilation/constriction of vessels, our immune system, and inflammation. There are more nerves in the gut than in the central nervous system, and many hormones that communicate between the gut and brain. Your gut not only influences mood—known as the gut-brain connection—but it also affects the nervous control of the heart and mediates some of the effects of stress on heart disease.
The gut interface
Did you know that bacterial organisms comprising our microbiome vastly outnumber our own cells? The variety of DNA in the microbiome far exceeds our own DNA. Considering the close cooperation of our physiology with that of the microbiome, there is ample opportunity for this relationship to go awry. This has implications for our regulation of cholesterol and metabolism.
Our gut represents the major interface between our insides and the outside world. So, our immune system, which protects us from outside world invasion, is heavily invested in protecting this interface. In fact, most of our immune cells are in the gut. Autoimmune dysregulation and inflammation present the opportunity for the development of heart disease. For a long time, we’ve known that plaque in the coronary arteries can harbor harmful bacteria and viruses. The inflammatory response from your body to these microorganisms can lead to plaque rupture—heart attack.
The role of your microbiome
Your microbiome has a prominent role in metabolism. The gut microbiome can increase estrogen levels by secreting B-glucuronidase, an enzyme that converts estrogens into active forms that can be reabsorbed back into the bloodstream. This can contribute to obesity, metabolic syndrome, and cardiovascular disease (CVD). In experiments on mice, the microbiome of obese and thin mice is so different that when we transplant the microbiome of the fat mouse into the thin mouse, the thin mouse becomes obese. Research on how the gut microbiome impacts our hormones, weight, and more is a burgeoning field of study.
Short chain fatty acids (SCFA) are produced when the gut bacteria ferment fiber, and affect appetite, insulin resistance, and cardiometabolic health. The three most common SCFAs are acetate, propionate, and butyrate. Butyrate is used as an energy source for colon cells and is important for colon health. This is one reason we recommend a whole-foods diet full of fiber, especially if you’re on a high-fat diet.
Bacteria in the gut produce TMA, a precursor of TMAO, a substance linked to heart disease. TMA is produced during the metabolism of choline, found in eggs, meat, and fish. The causative role of TMAO in heart disease is not established. But if the production of TMA is harmful, the solution may not be eliminating eggs meat and fish, but may be better accomplished by promoting a healthy microbiome with a diet rich in fiber and plant phytonutrients.
Intestinal permeability
Abnormal intestinal permeability, also called leaky gut, is a common condition that leads to inflammation and autoimmune responses that illustrate the link between the gut and heart disease.
Intestinal cells are designed to allow the passage of fully digested nutrients and to facilitate the transport of micronutrients into the bloodstream. In a healthy intestine, there is a barrier between the cells lining the gut that prevents partially digested proteins and pathogens from entering.
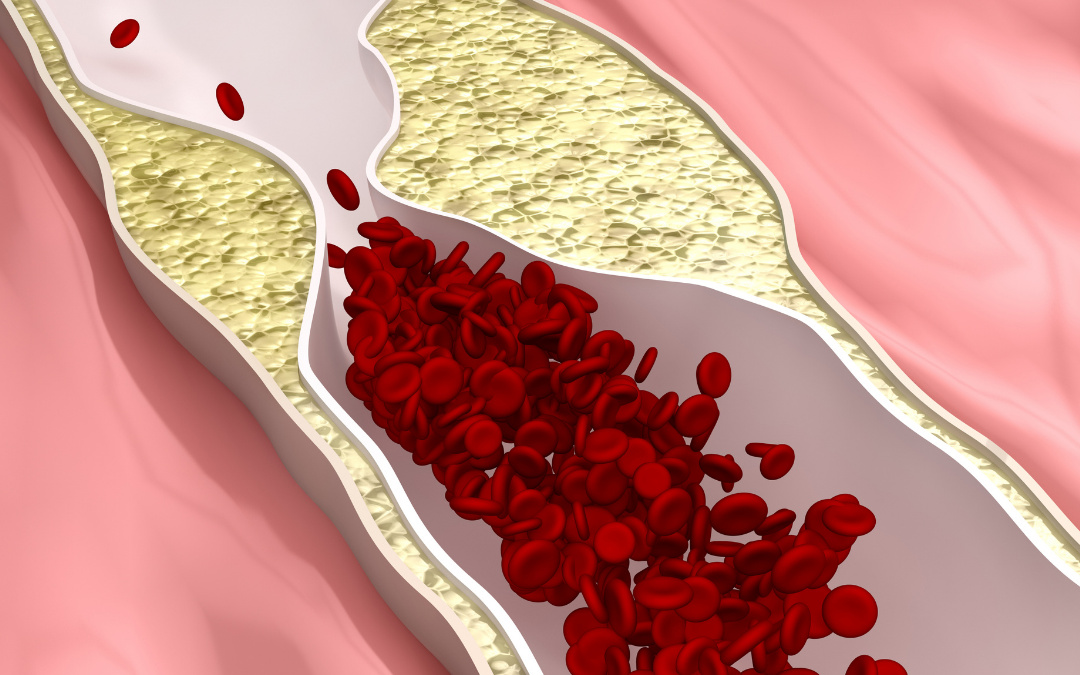
Leaky gut represents a breakdown of this barrier function. It begins with dysbiosis, damage to the mucosal layer above the intestinal cells, which can cause nutrient deficiencies. As the permeability progresses to tiny holes or tears, foreign substances escape your intestine. Your body creates an inflammation and immune response to neutralize the invasion. But when the leak is chronic or excessive, damage leads to elevation of cholesterol, atherosclerosis, and other forms of heart disease.
Metabolic endotoxemia occurs when lipopolysaccharide (LPS) fragments of bacteria enter the blood stream. These bacterial fragments are highly inflammatory. If food fragments enter your blood stream, your body’s antibody reaction to those fragments can create food sensitivities. These reactions can activate the immune system to react to and damage our own tissues, creating an autoimmune disease. Among other manifestations of heart disease, autoimmune processes are significant contributors to coronary artery plaque formation and plaque rupture.
Bacteria in the gut can affect cholesterol levels by breaking down cholesterol in the bile before it is reabsorbed back into circulation. Treating your leaky gut can have the same impact as taking statins for high cholesterol. The enzyme that increases cholesterol production, which statin medications block, is regulated by the gut. We can sometimes avoid prescribing a statin by correcting leaky gut and down-regulating enzyme and cholesterol production through diet and lifestyle changes.
Improving your gut health can also provide some of the benefits of beta blockers, commonly prescribed for high blood pressure.
Processed foods and lifestyle triggers
Processed foods, including grains, are a potent cause of leaky gut. Gluten is a particularly bad offender, as humans cannot actually digest gluten proteins. Grains like wheat also typically carry pesticides such as glyphosate, which damages the health of the microbiome. The sugar content of grains doesn’t help either: sugar and alcohol also contribute to leaky gut.
Other lifestyle habits, such as poor chewing, lack of exercise, stress, and sleep problems contribute to leaky gut. Antibiotics and toxins can also disrupt your gut’s normal functioning.
Testing for leaky gut and inflammation
We can test for abnormal intestinal permeability by looking for antibodies to actin and zonulin, proteins that maintain the intestinal barrier. We also measure antibodies to LPS to diagnose metabolic endotoxemia. Antibodies to wheat proteins can be measured to gauge how irritating gluten is to your gut. A PULS test is one way to measure the extent of vascular inflammation.
Food sensitivities are a clue to the presence of leaky gut, as are autoimmune problems. There are over 80 know autoimmune diseases and the prevalence of these problems is increasing. Many autoimmune diseases are more common in women.
Autoimmunity and heart disease treatments
All autoimmune diseases are associated with increased heart disease. Research has identified antibodies to many different cardiac structures. Autoimmune mechanisms have a role in arterial plaque formation and plaque rupture, as well as high cholesterol and atrial fibrillation.
You don’t have to have GI symptoms to have abnormal intestinal permeability. Our approach to functional treatment of heart disease always starts with a nutrient-dense diet to eliminate processed foods. When possible, we advise a diet with reduced or no inflammatory foods, especially dairy and gluten. To identify other food sensitivities, we may prescribe a short-term elimination diet. We focus on supporting good digestion through probiotics, prebiotics, stress reduction, sleep, exercise, and removing environmental toxins. We’ve seen evidence that probiotic and prebiotic fiber therapy reduces lipids and blood pressure.
Heart disease, and for that matter all chronic disease, stems from inflammation, oxidative stress, autoimmune mechanisms, and metabolic dysfunction. Because our gut and microbiome are a common source of these problems, it makes sense to look there first for the underlying causes of your heart disease. It’s crucial to reduce the harmful effects of sympathetic nervous system activation on the heart with good gut and microbiome health that promotes normal vagal tone.
Learn more: Click here to watch a recording of our recent webinar on the Heart-Gut Connection.
