Related Posts

ARE YOU DEFICIENT IN OMEGA-3 FATTY ACIDS?
Related PostsRecently,...

WILL FISH OIL HELP OR HURT YOUR HEART?
Related PostsOmega-3...
THE FUTURE OF PLAQUE IMAGING & DIAGNOSING CORONARY ARTERY DISEASE
Related PostsWhat is...
IS YOUR GUT THE CAUSE OF YOUR HEART DISEASE?
Related PostsAt...

ABLATION AND BEYOND FOR ATRIAL FIBRILLATION
Related PostsShould...

NATURAL WAYS TO DO WHAT STATINS DO
Related PostsStatin...
CARDIOVASCULAR DRUGS AND POTENTIAL NUTRIENT DEFICIENCIES
Related PostsCommon...
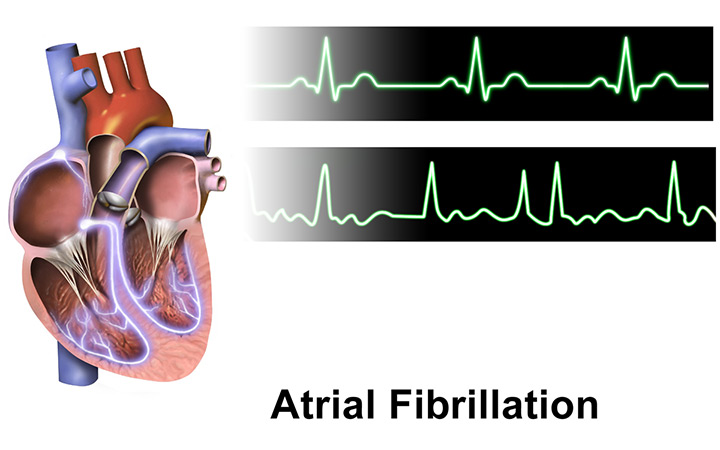
TREATING ATRIAL FIBRILLATION WITH ACUPRESSURE
Related PostsAtrial...

EARLY ABLATION FOR ATRIAL FIBRILLATION: IS IT BETTER THAN LIFESTYLE MODIFICATIONS?
In my previous blog post discussing ablation for atrial fibrillation, I recommend ablation as a tool for improving the symptoms caused by atrial fibrillation (AF), especially related to palpitations and exercise intolerance. Patients with weakened hearts do better and even live longer when ablation reduces the amount of atrial fibrillation they experience. But while it can reduce the symptoms, ablation only infrequently cures AF. Most people have some residual episodes. And over time, the benefit of ablation often diminishes.
In the big picture, ablation is a part of the treatment of atrial fibrillation in symptomatic people but does not stand alone as a cure. If you have AF, you want to determine the underlying causes and correct them.
Now there is the notion that “atrial fibrillation begets atrial fibrillation,” and if you provide a patient with the most effective therapy—ablation—early on, it will not progress to more prolonged, symptomatic, and complication-prone forms. I have even heard cardiologists suggest that ablation should be performed at the first sign of AF, to nip it in the bud, so to speak.
Unfortunately, I don’t think it is so simple.
Assumptions about atrial fibrillation progression
The rationale for early ablation stems from several hypotheses. First, that there is a gradual progression of AF from infrequent brief episodes to more frequent prolonged episodes, to persistence of the abnormal rhythm. The second hypothesis is that the cause of this progressive course is that the AF episodes themselves damage the atrium, making it increasingly prone to AF. The third hypothesis is that ablation can prevent most episodes of AF.
The problem is that each of these hypotheses are only partially true.
Does AF have a gradual progression?
Until 25 years ago, no one much cared about the natural history of AF. There was no effective way to help AF patients stay in normal rhythm. Doctors mostly ignored the condition until the prospect of performing catheter ablation for AF was developed. The tools to monitor patients’ heart rhythms for prolonged periods that we use today were not available. At that time, there was a presumption that AF starts as short infrequent episodes and gradually gets worse over time until it is present persistently. This presumption has not stood up to scrutiny. While some people follow a progressive course from infrequent to persistent AF, most don’t, and many start out with persistent AF without preceding brief episodes.
In a 2020 study that looked at the progression of atrial fibrillation in patients who did not receive an ablation, there was a lot a variability in the course of arrhythmia, with some patients getting worse, some getting better, and most staying the same.
On average, about 20% of people will progress from episodic paroxysmal AF to persistent AF over 5 years. About 40% of people seem to skip the paroxysmal AF experience entirely and present with persistent AF right off the bat.
Is AF the main cause of atrial damage?
The longer someone is in atrial fibrillation, the harder it is for them to get out and stay out. This is the source of the aphorism that AF begets AF. In experimental animals who are placed in AF by pacing the atrium at high rates, the longer they are paced, the more damage is seen in the atrium.
But in people, the exact damage to the heart that causes one person to have episodes of AF and another to have a persistently abnormal rhythm is poorly understood. In general, the degree to which the left atrium becomes damaged by the formation of fibrosis (scar tissue) is associated with more persistent AF. We can measure left atrial damage with MRI techniques, but these are hard to do and are rarely done. More commonly, the degree of damage is implied by enlargement of the left atrium on an echocardiogram and more accurately by changes in motion, which are termed left atrial (LA) strain. During an ablation procedure, abnormal electrical signals generated by the LA muscle can be measured and thus applied to the degree of LA damage.
Damage to the LA is important to know not just because it promotes more AF, but also because it makes people more prone to all the complication of AF, particularly clotting and stroke. Stroke with AF is very uncommon in people who have a perfectly healthy atrium, and strokes occur in people with a damaged atrium even if they don’t have AF! So, the health of your atrium is one of the most important things you can know if you have AF.
The contention is over whether AF itself is the main cause of damage to the LA or if it’s the other way around. This is a big and important distinction. Ablation is the most effective way to suppress AF symptoms. So, if AF is causing most of the damage, ablation should make a big difference in prognosis, not just of AF burden but of AF complications.
Does ablation reduce atrial damage?
Ablation can reduce the risk of progressing to persistent AF. In the recent ATTEST study, ablation was performed in patients with paroxysmal atrial fibrillation. After 3 years, very few of the ablation patients had persistent AF, compared to 17% in the control group. 83% of the control patients did not progress to persistent AF. 50% of the people in the ablation patients still had episodes of AF, but ablation did reduce the amount of AF and AF symptoms they experienced.
But the important question is whether the ablation reduced the damage to the atrium as well as the burden of AF. The ATTEST study did not measure this. So far, no studies have showed that ablation reduces the amount of damage to the LA. This is partly because that damage is difficult to measure and also because ablation, by its nature, increases the amount of fibrosis in the atrium. Ablation works by surrounding the pulmonary veins with scar tissue to prevent the initiation of AF by the emergence of electrical signals from the veins.
What else can cause atrial fibrillation?
Atrial fibrillation is not a single disease. People have AF with many different underlying problems that end up damaging the heart in ways that allow it to go into AF. But there is increasing evidence that for many people, the damage to the atrium is the initiating problem. There is evidence that AF is an inflammatory condition of the atrium brought on by a variety of possible insults and commonly the insult is the buildup of fat on the atrial surface. This epicardial fat is a source of inflammation and causes scarring in the adjacent atrial tissue.
Fibrosis is found in the atria of people who have new onset of AF, suggesting it is the cause of AF and not the result. Atrial fibrosis can also be seen in the atria of people at risk for AF but who have not yet had AF. Again, this suggests that the atrium is damaged before the arrhythmia begins.
In another study, an enlarged atrium predicted increased mortality even in people who have not had AF. AF can be an indicator that the atrium is damaged, but atrial damage does not always result in AF symptoms.
Severe or persistent atrial fibrillation burden may accelerate progressive damage to the LA in patients with AF, but it is not likely to be the sole cause. Reducing the burden of AF is not likely to reverse atrial myopathy when inflammation continues to cause damage.
Early lifestyle treatments for atrial fibrillation
Ablation is not a magic bullet. Ablation does not cure atrial myopathy. Ablation does not happen without substantial cost and the risk of rare but life-threatening complications. Ablation should not be recommended to minimally symptomatic people with the promise that it will cure AF and prevent future complications.
LA damage, also called atrial myopathy, is the real problem we need to treat, whether AF is present or not. AF certainly aggravates complications, perhaps by accelerating the damage to the LA and by reducing blood flow in the atrium. This makes your heart even more prone to clotting and stroke.
But there is no a treatment available to heal the left atrium. Or is there? There’s no pill, but lifestyle modification has shown to impact the natural history of atrial fibrillation and improve atrial myopathy.
In the ARREST-AF trial, patients had ablation either with or without the addition of a lifestyle modification program. These overweight patients went on a low-glycemic high-protein diet, exercised, received medical therapy as needed for blood pressure and lipid abnormalities, and got treatment for sleep disorders. Not only did the lifestyle patients have better outcomes from their ablation with less AF, but the lifestyle modification patients also had reduction in the size of their left atria. Weight reduction and better metabolic health reversed atrial myopathy compared to the ablation alone. Patients with ablation alone had no statistically significant reduction in LA size.
Another study, LEGACY, was an observational trial of weight loss in obese patients with AF. The degree of weight loss related not only to the degree of improvement in AF burden without ablation, but it also resulted in reduction of LA size.
In obese animals, weight reduction reduces the epicardial fat that accounts for the electrical abnormalities that promote atrial fibrillation.
Find and treat the root causes of your AF
There is not a new reason to have an ablation for new-onset atrial fibrillation. But there is a powerful reason to identify and treat the underlying cause of left atrial myopathy. Our goal should be to improve the results of ablation and even eliminate the need for ablation in some people. To do this, our therapy targets should focus on lifestyle and metabolic health: get rid of inflammatory visceral fat; reduce autoimmune reactions through dietary changes; reduce toxin burden; and address disordered sleep and chronic stress.
By addressing the underlying causes of AF, we can hope to need fewer ablations, not more. Instead of early ablation for your AF, try early application of lifestyle changes.
Learn more:
Try this at-home acupressure technique for AFib symptoms
