
Related Posts

WILL FISH OIL HELP OR HURT YOUR HEART?
Related PostsOmega-3...

EARLY ABLATION FOR ATRIAL FIBRILLATION: IS IT BETTER THAN LIFESTYLE MODIFICATIONS?
Related PostsIn my...
THE FUTURE OF PLAQUE IMAGING & DIAGNOSING CORONARY ARTERY DISEASE
Related PostsWhat is...
IS YOUR GUT THE CAUSE OF YOUR HEART DISEASE?
Related PostsAt...

ABLATION AND BEYOND FOR ATRIAL FIBRILLATION
Related PostsShould...

NATURAL WAYS TO DO WHAT STATINS DO
Related PostsStatin...
CARDIOVASCULAR DRUGS AND POTENTIAL NUTRIENT DEFICIENCIES
Related PostsCommon...
TREATING ATRIAL FIBRILLATION WITH ACUPRESSURE
Related PostsAtrial...

ARE YOU DEFICIENT IN OMEGA-3 FATTY ACIDS?
Recently, I wrote about the problems with using fish oil as a medication. What does it look like if we view fish oil supplementation not as a heart drug, but through the lens of replacing a deficiency?
We’re short on omega-3s
There is a lot of evidence that most Americans are deficient in omega-3 fatty acids. We measure levels with a test called the Omega-3 Index. The index measures the percentage of EPA and DHA phospholipids in red blood cell (RBC) membranes. We can also measure omega-3 levels directly in the blood, but the level changes based on what you ate before the test. An Omega-3 Index level of 3% is low; 5% is typical for Americans. An index of 9% is typical of populations like Japan where fish consumption is high, and 8% would be a practical target goal.
Why measure omega-3 fatty acids? Because there is a strong relationship between these levels and health outcomes.
Baseline Omega-3 Index, in people without supplementation, correlates with all-cause mortality, as well as cardiovascular mortality. In the Framingham Study cohort there was a 5-year difference in age at death between the people with the lowest Omega-3 Index, around 4%, to the highest, around 7%. A low Omega-3 Index was equal to smoking as a predictor of mortality.
Dolphins max out at an Omega-3 Index of 18%, and they eat only fish. So, at some point the cell membrane, where omega-3 fatty acids are stored, has the optimal amount of EPA/DHA, and taking more doesn’t help. That is why I suspect that health depends not on filling the blood with pharmaceutical levels of EPA/DHA (such as when omega-3s are prescribed) but on restoring the correct balance of EPA/DHA in the cell membranes.
What’s on your plate?
Americans eat 13 pounds of fish per year, on average. Most of that is white fish like pollock, which is found in fast food fish sandwiches. Pollock is very low in omega-3 fatty acids, as are shellfish. Salmon and sardines contain 1 gram of EPA/DHA or more in a 3.5 ounce (100 gram) serving. Half of Americans have no EPA/DHA intake. Overall, Americans eat a daily average of around 150 mg of omega-3s (mostly ALA), while the typical person in Japan consumes 900 mg per day. Japan’s average lifespan is five years longer than in the US, despite higher stress levels, higher smoking rates, and a higher incidence of hypertension.
How omega-3s act on your cells
We always discuss fish oil in terms of reducing inflammation or causing bleeding. This may be backwards thinking. Maybe we have high inflammation and increased clotting because we are deficient in omega-3 fatty acids to begin with.
The omega-3 fatty acids in cell membranes are used to make compounds that both initiate and resolve inflammation. Fish oil supplements correct this deficiency, restore the balance, and reduce inflammation in someone who is deficient. But we should not expect excessive amounts of omega-3 fatty acids to provide more benefit if your Omega-3 Index is normal.
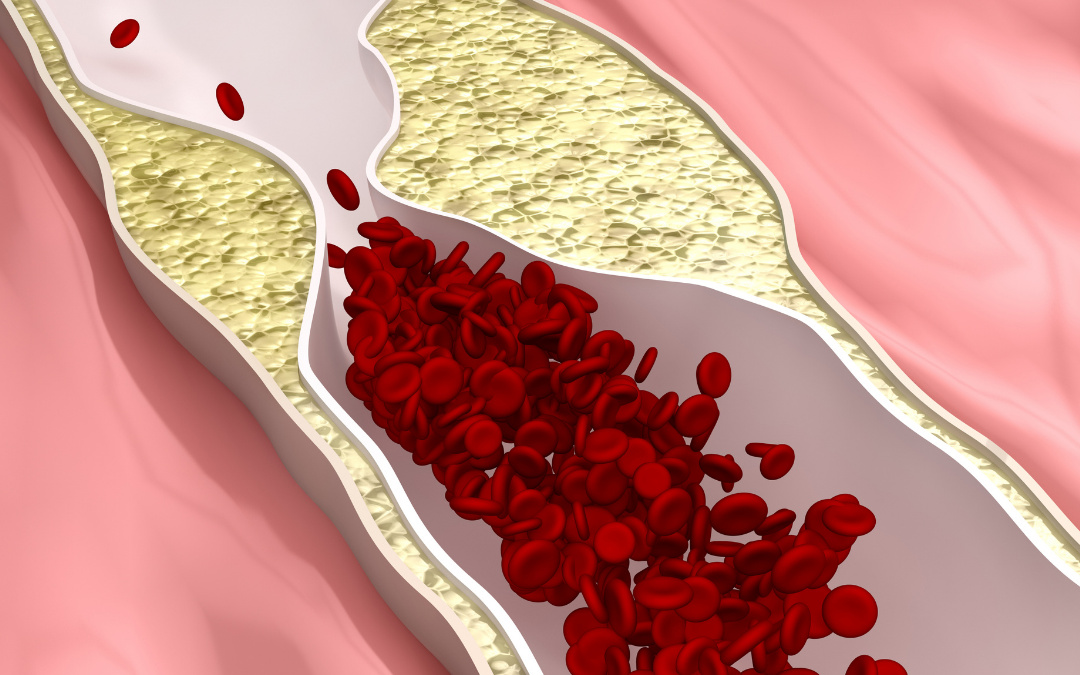
Omega-3 fatty acids in the cell membranes of platelets regulate platelet aggregation, a mechanism involved with blood clotting. Fish oil is known to increase bleeding time, but studies have not demonstrated abnormal bleeding with fish oil supplementation. This suggests that people with a low Omega-3 Index have abnormally increased clotting, and fish oil supplementation restores the normal balance between clotting and bleeding.
(Note: due to the increase in bleeding time, your doctor may ask you not to take fish oil supplements before a surgical procedure. Humor them.)
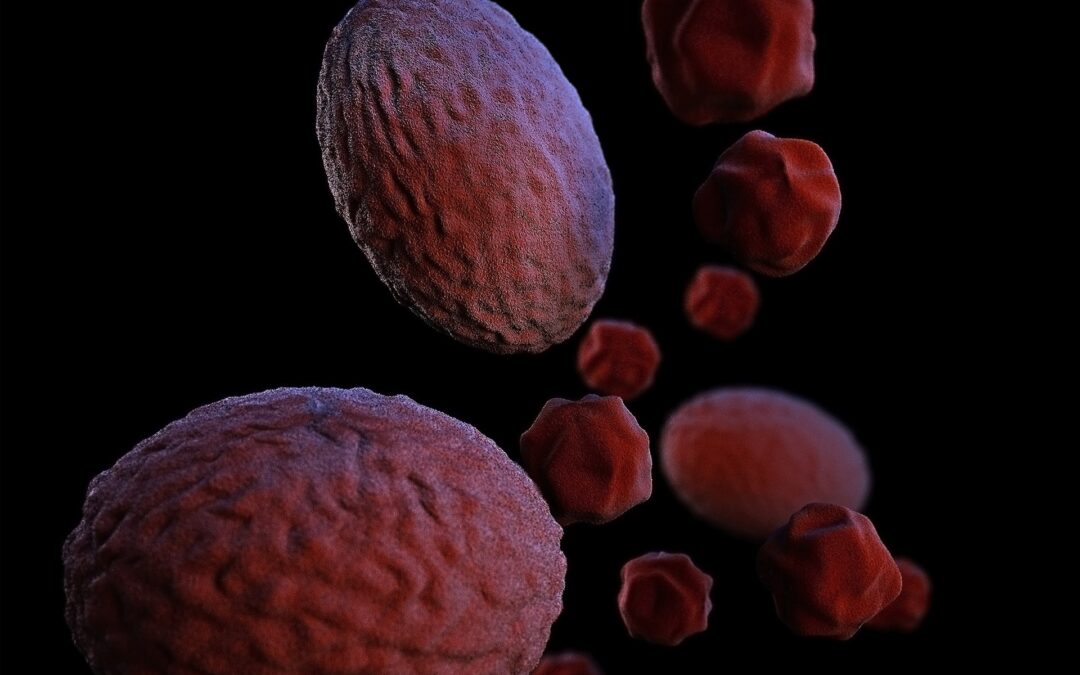
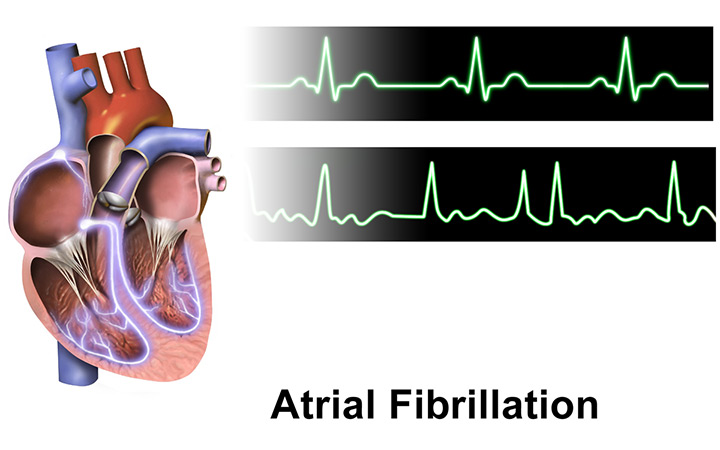
The percentage of EPA/DHA in cell membranes determines how fluid and flexible the cell is. People with a low Omega-3 Index have red blood cells that vary in size, shape, and deformability. A complete blood count test (commonly done with any labs at your doctor’s office) measures RDW, or red blood cell distribution width. People with a low Omega-3 index have higher RDW, more inflammation, higher rates of cardiovascular and cerebrovascular disease, and more complications from hypertension and atrial fibrillation. Restoring the fluidity of red blood cells can improve delivery of oxygen to tissues, but, again, taking extra is not likely to be helpful.
While EPA/DHA is often recommended or prescribed for high triglyceride levels, the benefit of supplementation is likely confined to people with low Omega-3 index and results from correcting the inflammation, atherogenic lipoproteins, abnormal clotting, and abnormal cell fluidity that omega-3 deficiency causes.
Dietary sources of omega-3 fatty acids
There are three omega-3 fatty acids: alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). They are essential, meaning we must get them from dietary sources. ALA, which we get from nuts and seeds, has different physiologic effects than EPA/DHA, which are found in fish, seaweed, and algae.
Fish and fish oil are the most common sources of dietary and supplemental EPA/DHA. Fish don’t make EPA/DHA; they get it from eating algae.
Diet is clearly the best way for us to get omega-3 fatty acids. One of the few things that epidemiology studies show with consistency is the benefit of regularly consuming fish. A serving of omega-3 fatty acid-rich fish, such as salmon, sardines, and mackerel, will supply at least 1 gram of EPA/DHA. By comparison, supplement doses of EPA/DHA range from 840 mg to 4 grams per day.
How do you know If you are getting enough?
It makes sense to intake more omega-3 fatty acids if you are deficient. So, how do you know If you’re deficient?
If you have an omega-3 fatty acid-rich diet but are dealing with heart disease, you should consider measuring your Omega-3 Index. We use this test to detect deficiency, motivate supplementation, and verify the effectiveness of your diet or supplementation.
You can have your Omega-3 Index measured in several ways. One convenient way that you can measure for yourself is through a company called OmegaQuant, based in South Dakota. For $49.95 they will mail you a card, you prick your finger to provide a blood sample, and mail the card back in.
If your omega-3 levels are good, you don’t need to change. Taking supplements is tedious and expensive, so only take what you know you need.
If you are supplementing and have a low level, you may need more or you may need to make other lifestyle changes. Response to dietary or supplemental Omega-3 fatty acids varies a lot, and one factor is GI (gastrointestinal) absorption. Improving your gut health and microbiome may improve your absorption of omega-3s.
What I do for heart health
I don’t take fish oil as a therapy for heart disease, but I do take it to be sure I am not deficient. I eat wild salmon once or twice a week. I love it grilled, steamed, or smoked. Beth likes to dress it up with interesting sauces or rubs (try her delicious recipe for One-Pan Mediterranean Baked Fish). Canned sardines and mackerel are a convenient add-on to a salad. I supplement with 1-2 grams of EPA/DHA most days as well. This provides a normal Omega-3 Index for me. My atrial fibrillation has not been improved or aggravated by fish oil, but you need to be vigilant for any side effects. You may be interested to follow your hs-CRP, TG/HDL levels, and RDW to see If they improve from eating more fish or supplementing with fish oil.
